In 1995, stent implantation became the second revolution in interventional cardiology when Colombo et al. demonstrated that intravascular ultrasound (IVUS)-guided post-dilatation of stents to achieve optimal expansion and larger lumens led to reduced restenosis and stent thrombosis (ST).1 This ‘bigger is better’ hypothesis became the technical cornerstone of all stent implantation in the bare metal stent (BMS) era. Despite numerous smaller randomised studies demonstrating superiority of IVUS over angiography in diagnosing suboptimal stent expansion and thereby resulting in improved outcomes,2 most operators – in the absence of IVUS guidance – made it a uniform practice to post-dilate stents to achieve an angiographic ‘step up and step down’ appearance. The initial hype of dramatic reduction in restenosis and target lesion revascularisation (TLR) with drug-eluting stents (DES) led to a false belief that the ‘bigger is better’ hypothesis was redundant and that post-dilatation was an unnecessary for DES. However, it was soon realised through IVUS-guided studies that one of the strongest predictors of restenosis, target vessel revascularisation (TVR) and ST – even with DES – was suboptimal stent expansion and minimal stent area (MSA).3,4
While it is clear that post-dilation with a non-compliant (NC) balloon can optimise stent expansion and achieve larger stent areas, there are no major randomised studies to prove that this translates into improved hard endpoints of major adverse cardiac events. Postdilatation could also possess inherent disadvantages and cause complications, which may outweigh its benefits. Furthermore, the current generation of stent delivery balloons are less compliant, allowing higher-pressure implantations. Hence, post-dilatation in the present DES era is variable and has been left to operator experience and discretion. Many operators deploy the stent with the implantation
balloon to moderate pressures of 12–16 atmospheres and occasionally to higher pressures of 16–20 atmospheres. Others prefer to postdilate after moderate pressure implantation with an optimal size or quarter size larger NC balloon to 16–20 atmospheres based on angiographic guidance. A minority do this post-dilation selectively under intracoronary imaging guidance.
The Need for Post-dilatation
Twenty to thirty per cent of stents are found to be under expanded on IVUS in various studies of both BMS5,6 and DES7 after standard deployment with stent balloons. Costa et al. studied second-generation BMS and found that in vivo only 3.8 % of stents achieved >90 % of the nominal stent diameters as per recommended charts and that 70 % of stents were <80 % of the nominal diameter.5 The same was also true for DES.8
Suboptimal stent implantation is the result of an interplay of multiple factors in isolation or combination. These may include stent under sizing, compliance of the balloon and deployment pressures (the compliance charts from the manufacturer are in-vitro measurements that differ from what occurs in an atherosclerosed rigid coronary artery) and plaque vessel compliance (large plaque burden, calcium or fibrosis).
Suboptimal stent deployment may occur because of under sizing of the stent delivery balloon related to the target vessel. In this case even higher pressures on the semi-compliant balloon may not compensate for under sizing inside the vessel. Furthermore, pressures may not build up uniformly throughout the balloon length, especially when more outward force is needed at the area of maximal stenosis where there is the largest and most resistant plaque bulk. The semicompliant stent balloon – especially in large plaque burden, calcific or fibrotic lesions – does not achieve focused force at the lesion site, and at higher pressures results in ‘dog boning’ leading to underexpansion.
In the Stent Optimization (STOP) study, only 21 % of DES achieved optimal deployment at 16 atmospheres, which increased to 54 % after routine post-dilatation with an NC balloon to 20 atmospheres. Further IVUS-guided optimization achieved optimal deployment in 81 % of the stents finally.9 The Postdilatation Clinical Comparative Study (POSTIT)10 demonstrated that high-pressure stent deployment alone reaches only 55 % of the achievable luminal gain, whereas adjunctive NC balloon post-dilatation can double the frequency of optimal stent expansion. In a study of first-generation DES, follow up demonstrated that under-deployed stents with a cross-sectional area (CSA) <5–5.5 mm² was one of two procedural factors associated with restenosis, while a smaller area of 4.2–4.65 mm² was associated with ST.3, 11–13 DES with a larger CSA also have a more complete neointimal coverage.14 However, despite achieving optimal stent expansion and large CSA by IVUS guidance, many post-dilation studies have failed to demonstrate clear long-term benefits in outcomes.15 One important reason for this could be that the outcome benefits could be more demonstrable in high-risk subgroups such as calcified vessels, long lesions, fibrotic lesions, bifurcation lesions or ostial lesions, but these studies were underpowered to look at these subgroups.
We should also keep in mind that target vessel failure and ST are multi factorial. Refinements in stent materials and design, thinner struts, safer polymers, and better antiplatelet agents have all led to improved outcomes with present generation DES.
Nevertheless, the target vessel failure and ST rates are not insignificant. It is possible that the current generation of advanced thin-strut DES may possess lesser radial strength and thus excessive recoil, especially in complex lesions, thereby predisposing to smaller CSAs. It is therefore likely that the need for post-dilation with an NC balloon may be even more important in the present thin strut DES era.15
Rationale for Using NC Balloons for Post-dilatation
Romagnoli et al.15 demonstrated the advantage of achieving better stent expansion using NC balloon post dilatation over semi compliant stent balloons despite achieving the same final balloon size (based on manufacturer’s balloon compliance charts). The NC balloons not only have a linear relationship between the changes in applied pressure and the changes in observed volume (ΔV/ΔP, the definition of compliance) but also tolerate 50 % greater inflation pressures. These combined properties allow greater forces to be applied focally without overstretching other parts of the diseased segment.16 Atherosclerotic coronary artery distensibility by balloon inflation is a linear function of pressure at low inflation pressures only and primarily in arteries with concentric lesions.17 At higher pressures, of relevance for percutaneous coronary intervention (PCI), distensibility is unpredictable. De Ribamar Costa Jr et al.5 showed that stent balloon compliance charts overestimate the final stent dimensions, as these measurements are typically made in vitro without the vessel constraint that limits balloon expansion. When the stent is deployed at high pressures with the semi-compliant stent balloon, it may cause stent edge dissection, coronary perforation and intimal injury leading to an increased inflammatory response and higher restenosis rate.18 Hence, using an NC balloon for high-pressure post-dilatation stent optimisation is not just physiologically appropriate but technically safer than going up to higher pressures with a compliant balloon.
Disadvantages of NC High-pressure Post-dilation
While it has been clearly demonstrated that high-pressure postdilatation with the NC balloon helps optimise stent expansion and achieve a large lumen, disadvantages to the approach may also exist. Aggressive post-dilatation might result in more intimal hyperplasia compared with a less aggressive approach,19 or lead to edge dissections, geographic miss20 or even coronary perforation.21 These complications may require additional stenting and influence TLR adversely. Another possible complication of repeated recrossing of partially deployed stents with NC balloons is the risk of damaging the stent and causing longitudinal stent deformation, especially with newer generation thin-strut stents.22 High-pressure NC balloon postdilation may be associated with greater side branch occlusions and myocardial injury23 and may also be a risk factor for stent fracture and restenosis.24 During angioplasty in acute myocardial infarction, there is a thrombotic milieu and aggressive post-dilatation may lead to distal embolisation25,26 and ‘slow flow’ due to microvascular plugging and worsening myocardial damage.24 We should also not forget that post-dilatation adds to the cost of the procedure, which is an important consideration for many centres and countries across the world.
In The Real-World Endeavor Resolute Versus Xience V Drug-Eluting Stent Study in Twente (TWENTE) trial, post-dilatation was performed in 82 % of stents. This may have contributed to a higher incidence of peri-procedural myocardial infarction (4.1 %), although the 12-month clinical TLR rates were lower (2.1 %) compared with historic controls.27
In an analysis of more than 90,000 stent implantations from the Swedish Coronary Angiography and Angioplasty Registry from 2008 to 2012, Fröbert et al.28 looked at outcomes related to different implantation pressure and found that the risk of ST and restenosis appeared to be high with low (<15 atmospheres) and with very high (>20 atmospheres) pressure group.
Post-dilation in Bioresorbable Vascular Scaffolds
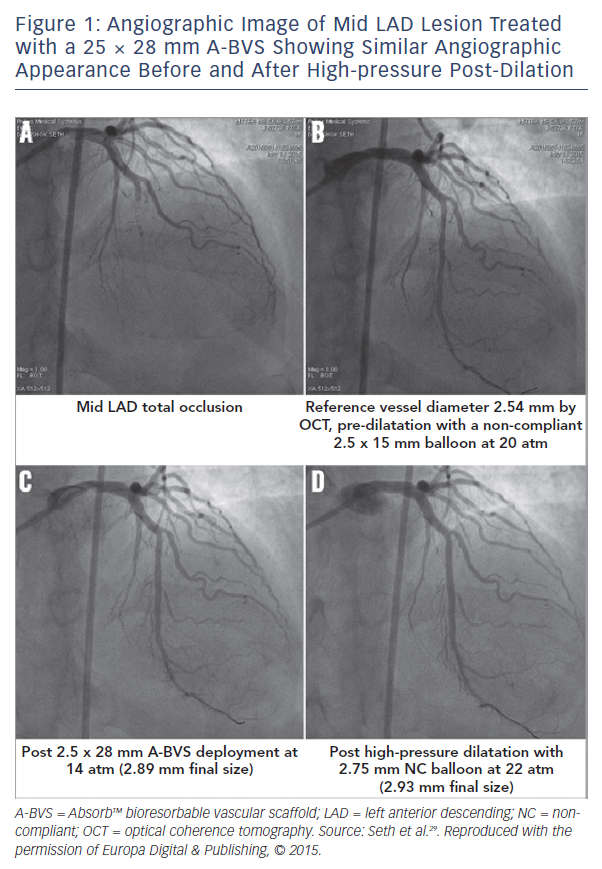
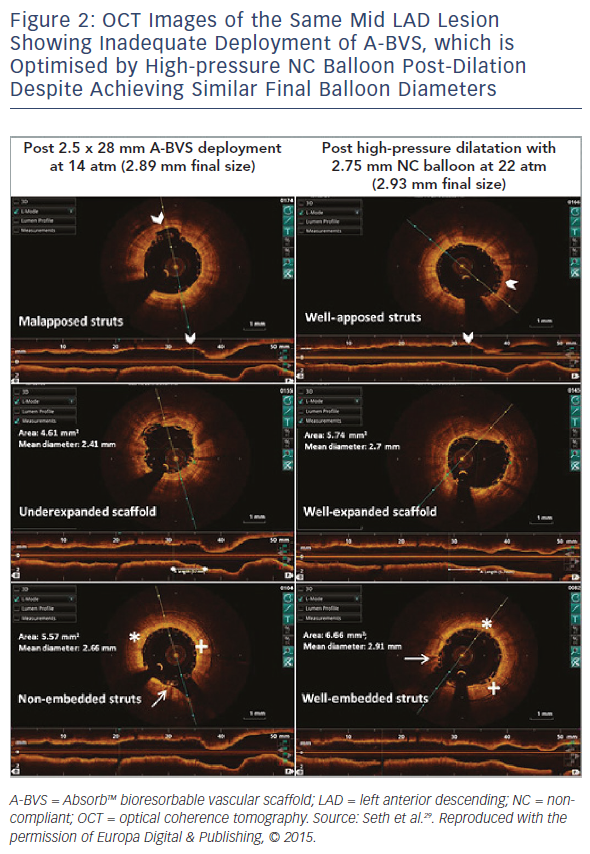
Bioresorbable vascular scaffolds (BVS) are thick-strut (156 μm) devices compared with current-generation DES, and in many ways similar to the first generation of metallic thin strut DES (65-85 μm). Over the last 3 years, the technique for optimal implantation of BVS has evolved to mandate the need for high-pressure post-dilation with a NC balloon. This achieves large MSA and also embeds the struts.29 The earlier studies of BVS, (Absorb II30 and Absorb III31), did not utilise high-pressure post-dilation with the NC balloon and deployed the scaffold at low to moderate pressures with scaffold balloon, which may have accounted for higher scaffold thrombosis rates at follow up. Registries and single-centre experiences using high-pressure NC balloon post-dilatation demonstrate outcomes as good as the bestin- class DES with extremely low scaffold thrombosis rates, although a randomised trial is still awaited on the impact of optimal implantation technique on the outcomes of BVS. However, through observations and experience, IVUS- or optical coherence tomography (OCT)-guided data from experienced centres it is now mandatory that for safe and effective implantation of BVS, the lesion should be prepared well, the BVS should be sized appropriate to the vessel and post-dilatation with a 0.25–0.5 mm larger NC balloon at 18-20 atmospheres keeping within the limits of scaffold expansion should be used. This help achieves the best outcomes.32
We have demonstrated by OCT that – despite adequate and aggressive pre-dilatation of the lesion and subsequent deployment of BVS to achieve a good angiographic result – a high-pressure post-dilatation with an NC balloon 0.25 mm larger (while achieving the same final size as the BVS implant balloon as per pressure compliance data chart) still corrects underexpansion, apposes struts, achieves better luminal enlargement and even embeds the thick struts into the vessel wall. All of this could help decrease ST and improve outcomes (see Figure 1 and Figure 2).29
Specific Conditions
Bifurcation lesion treatment is associated with a high incidence of non-uniform stent expansion especially in the side branch, resulting in a higher TVR rate.33 Several studies have demonstrated that when both branches are stented, final post-dilatation with a kissing balloon is associated with more favourable long-term outcomes.34–36. and is therefore mandatory.
In long lesions, the Randomised Trial of Endoluminal Reconstruction Comparing the NIR Stent and Wallstent in Angioplasty of Long Segment Coronary Disease (RENEWAL) and Multicenter Ultrasound Stenting in Coronaries (MUSIC) studies showed that high restenosis rates with long stents could be related to suboptimal stent deployment.37 Thus, for long or overlapping stents, high pressure NC balloon post dilatation especially at the overlapping zone achieves maximal luminal gain as well as optimally apposes the double layer of stents. so that struts are properly apposed to wall in double layer of stents.
Ostial lesions are usually fibrotic and resilient, and there is expert consensus to post-dilate the stents with a NC balloon to enable optimal expansion.
Conclusion
Advancements in science, technology and drugs have improved outcomes of stent implantation. At the same time more complex patient and lesion population are being increasingly treated. Thus, improving on target lesion failure rates and ST remains an important focus. Even the current generation of DES need a perfect final result and technique continues to play an important role. With multiple tools at our disposal, lesion evaluation and result optimization by IVUS or OCT, vascular bed preparation and plaque modification with scoring/ cutting balloons or rotational atherectomy, achieving end-to-end lesion coverage and avoiding geographical miss are important for long-term outcomes. Finally, post-dilation continues to play an important role for achieving maximal luminal gains.
It is highly unlikely that any large randomized trial will be performed to test the concept of high-pressure post-dilatation of DES in current era and frankly we don’t believe such trials are needed. Achieving complete stent apposition and maximal luminal gain still remains the ultimate goal and is associated with the best long-term outcomes. Not all lesions in our PCI practice require post-dilation with NC balloons. Type-A denovo lesions, lesions in large vessels >3.5 mm or softer lesions could achieve a large CSA even with the current generation of semi-compliant stent implantation balloons. However, more than 60–70 % of the lesions we treat in real-world practice include bifurcation lesions, ostial lesions, left main lesions, calcified or fibrotic vessels, small vessels, in-stent restenosis, overlapping stents or tapering vessels. These lesions have higher thrombosis and restenosis rates and follow up. High-pressure post-dilatation of DES in these complex lesions should be considered standard practice preferably with intracoronary imaging to achieve the best outcomes in the short and long term.