Dr Baldetti’s talk covered the importance of the correct positioning of Impella implantation to avoid device-related complications and to optimise its function. In his presentation, Dr Baldetti discussed how correct positioning is best achieved, and presented results from his study to improve assessment of Impella malrotation.
Dr Baldetti set out the three conditions that need to be met in order to achieve correct positioning of the Impella on implantation. The first condition is correct positioning represented by the waveforms on the device console; the second is the correct shaft depth across the aortic valve; and the third condition requires the pigtail to be directed downward towards the left apex and away from the lateral left ventricle (LV) wall. Correct Impella positioning is only fully fulfilled when all three conditions are met. The gold-standard method to assess correct Impella positioning is transthoracic or transoesophageal echocardiography; however, these methods are not always used in clinical practice.
Dr Boldetti explained that if only the first two conditions are fulfilled, this can result in Impella malrotation, and this is thought to occur in as many as 32% of cases. Compared with no malrotation, device malrotation is associated with higher rates of adverse in-hospital outcomes, including higher degrees and worsening degrees of aortic regurgitation during support (14.7% versus 68.8%; p<0.001) and an increase in MI (0% versus 12.5%; p=0.035), major bleeding (14.7% versus 43.8%; p=0.025) and stroke (0% versus 12.5%; p=0.035) while in hospital.1 However, Impella malrotation is not easy to detect relying on 2D fluoroscopy imaging alone because these images lack anatomical landmarks and do not provide clear visualisation of the LV apex. Therefore, there is a need for a standardised fluoroscopic protocol for assessment of device malrotation on implantation.
Dr Baldetti presented his centre’s methods to achieve this aim. A patient with a malrotated Impella underwent a contrast-enhanced multidetector non-ECG-gated chest CT scan during Impella support, and the images were compared with those of a patient with a correctly positioned Impella. The CT scans provided imaging of the direction and location of the device that matched three- and four-chamber echocardiogram views. Although Dr Baldetti recognised that different imaging modalities methods can offer different implant views, he rationalised the choice of CT scans because they provide volumetric data, angulation reconstruction and can be translated to match fluoroscopy imaging.
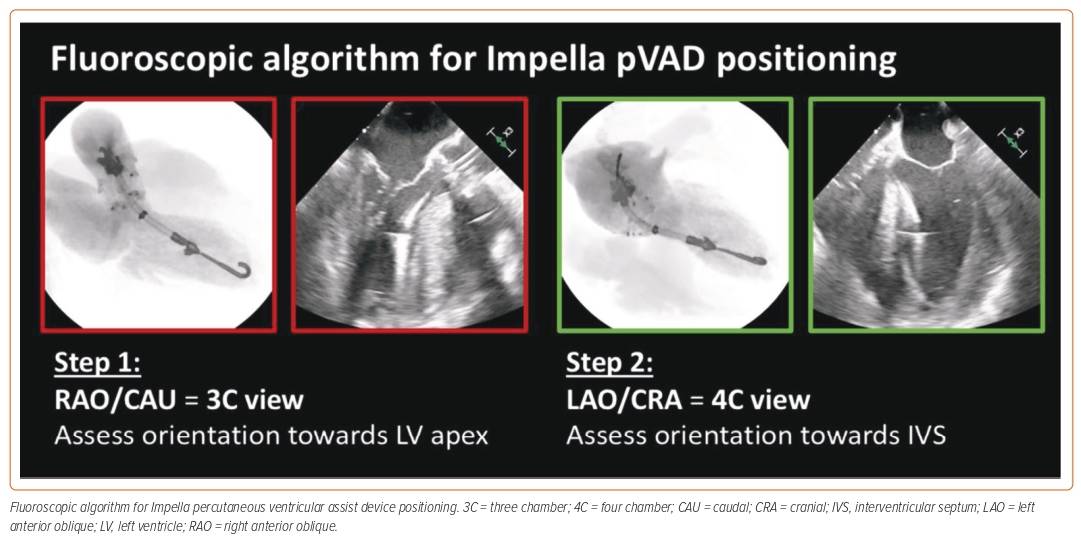
Dr Baldetti identified the mitral valve annulus as the most suitable anatomical landmark to rely upon to guide assessment of implant positioning and noted that it can be lined up with the Impella, using its ring as the marker. He applied the S-curve method to assess optimal implant views.2 By using a multiview approach, Dr Baldetti demonstrated that it is possible to assess the orientation of the Impella towards the LV apex, the depth of the device across the aortic valve and the laterality of the device (Figure 1).
Dr Baldetti provided the results of his proof-of-concept validation case that tested this approach in a real-world setting, which confirmed the device was appropriately positioned. The position was verified to be correct by ECG performed in the intensive care unit. Dr Baldetti concluded that the fluoroscopic implant approach for Impella allows for rapid assessment of pump positioning and may overcome the lack of ultrasound imaging availability in centres. The right anterior oblique and caudal views may present the preferred implant fluoroscopic views, whereas multiple views may further refine assessment of device orientation within the LV. Dr Baldetti acknowledged that this approach was validated in only one patient; further validation is underway.