Stent failure (SF) is a widely used term enveloping the aetiologies of in-stent restenosis (ISR), stent thrombosis (ST) and stent fracture (StF). The mechanisms of each vary: ISR is most commonly secondary to neointimal hyperplasia or neoatherosclerosis; ST is often precipitated by malapposition and incomplete stent strut coverage; and StF, although much rarer, is caused most frequently by vessel motion at hinge points. In addition to these factors, a number of patient comorbidities, as well as coronary lesion characteristics, procedural strategies and stent design factors, increase the risk of SF. Despite the evolution of stent platforms and increasing adoption of precision percutaneous coronary intervention (PCI) facilitated by adjunctive calcium modification and the use of intracoronary imaging, SF poses an ongoing challenge to coronary revascularisation. Although the shift from bare-metal stents (BMS) to drug-eluting stents (DES) saw a decrement in overall ISR rates, ISR remains the primary culprit for failure of contemporary PCI.1
Target lesion revascularisation (TLR) rates of between 3% and 20% are consistently reported across randomised controlled trials (RCTs) and large registries, regardless of the coronary vessel treated, lesion complexity or the use of image-guided stent optimisation.2–5 In both the EXCEL and NOBLE trials, with >70% uptake of intravascular ultrasound (IVUS) for left mainstem PCI and the use of DES, TLR rates of approximately 12% were reported.6,7 Similar trends have been seen in trials of coronary artery bypass grafting (CABG) versus PCI incorporating complex multivessel coronary disease and diabetic cohorts, proven to be at increased SF risk, with TLR rates of 19% in the SYNTAX trial at the 5-year follow-up, 5.7% in the BEST trial and 12.6% in the FREEDOM trial.8–10
ISR and TLR are also common phenomena following PCI for chronic total occlusion (CTO), a challenging subset of coronary disease, the treatment of which frequently induces greater vessel trauma. In the ACE-CTO study of 100 patients following implantation of second-generation everolimus-eluting stents (EES), the 12-month TLR rate was 37%.11 However, significantly lower TLR and target vessel revascularisation (TVR) rates have been shown in both RCTs and registries. For example, an evaluation of long-term clinical outcomes following CTO PCI in three tertiary centres found TLR and ST rates of 17.2% and 1.7%, respectively, with use of DES.12 More recently, the CONSISTENT CTO study found TVR rates of 4.8% and 17% in non-diabetic and diabetic cohorts, respectively.13 Although earlier data, such as those from the J-Cypher 5-year outcomes study, demonstrated higher rates of TLR in CTO PCI versus unselected non-CTO PCI, more recent data directly comparing outcomes of CTO PCI versus complex non-CTO PCI found equipoise in target vessel failure (TVF) at the 3-year follow-up.14,15 This was despite higher cardiovascular comorbidity, a lower degree of procedural success and higher complication rates in the CTO treated cohort.
The aim of this review is to provide a structured and comprehensive summary of the primary factors influencing and predicting SF (Figure 1), primarily ISR, in the CTO population, alongside strategies to mitigate these.
Patient-related Factors
Numerous comorbidities and clinical entities increase the absolute risk of SF secondary to ISR and ST. In this review, we focus on diabetes, chronic kidney disease (CKD) and dyslipidaemia.

Diabetes
Diabetes is prevalent in approximately 40% of patients undergoing CTO PCI and is an independent predictor of ISR.16 Intimal hyperplasia is promoted by vessel trauma during stenting, and the effects of hyperinsulinaemia on smooth muscle cells, leading to luminal loss, reduced minimal luminal area and subsequent TLR/TVR.17 A 980-patient single-centre observational study comparing outcomes in diabetics with HbA1c <7% versus >7% showed increased major adverse cardiovascular events (MACE), driven primarily by repeat revascularisation, in those with poorer glycaemic control (TLR and non-TLR).18 These findings are echoed in other large studies and a meta-analysis demonstrating trends towards increased ISR and TLR in diabetic cohorts with a higher HbA1c or glucose level at index PCI, with increasing severity of disease predicting increased TLR in a stepwise manner.19,20
Furthermore, one large study showed TVR rates to be significantly increased in diabetic patients with poor glycaemic control compared with non-diabetic patients, whereas in diabetic subjects with good glycaemic control the outcomes were equivalent to those in a non-diabetic matched population, reinforcing the importance of vigilant glycaemic management.21 Similar findings were observed in the CONSISTENT CTO study, in which TVR rates were significantly higher at both 12 months (15.9% versus 4.8%) and 2 years (27.3% versus 7.8%) in diabetic versus non-diabetic cohorts undergoing CTO PCI.13
Chronic Kidney Disease
Almost 30% of patients undergoing CTO PCI have Stage III CKD, defined as an estimated glomerular filtration rate (eGFR) <60 ml/min/1.73 m2, either as an end-organ manifestation of diabetes or hypertension or secondary to alternative renal or systemic pathology.22 CKD is associated with accelerated and aggressive atherosclerotic coronary disease, increased MACE (including post-coronary revascularisation) and higher SF rates. Mechanisms linked to conventional coronary risk factors include activation of the renin–angiotensin–aldosterone system in hypertensive patients, increased insulin-like growth factor in diabetic patients and malignant patterns of dyslipidaemia, including upregulation of LDL receptor expression and increased triglyceridaemia. Furthermore, higher levels of novel coronary risk factors, including homocysteine and certain forms of apolipoprotein, have been consistently found in CKD patients alongside increased oxidative stress and reductions in endothelial nitric oxide levels (crucial for vascular integrity).23
Trials in coronary intervention frequently exclude CKD patients, 80% excluding end-stage renal disease and 60% excluding any CKD, due to the challenges of revascularisation in these patients resulting from increased coronary calcification and the need to minimise contrast load.24 In a pooled analysis of over 12,000 patients in the Korean Multi-Center DES registry, TLF was significantly higher in the CKD versus preserved renal function cohort, with a trend towards increased ST at 30 days.25 In the Japanese Multicentre Prospective Registry outcomes analysis of 4,749 patients, an eGFR <30 ml/min/1.73 m2 and haemodialysis dependence were associated with reduced procedural success (primarily due to failure of retrograde wire cross), higher in-stent occlusion rates (p<0.001), increased lesion calcification, proximal tortuosity and occlusion length >20 mm, and subsequently higher J-CTO scores.26 Further, dialysis dependence was a predictor of 12-month major adverse cardiovascular and cerebrovascular events driven by death, TVR and CABG.26 An eGFR <40 ml/min/1.73 m2, alongside diabetes, left ventricular (LV) ejection fraction <45%, volume-deplete hypotension, increasing age and anaemia, predicts an increased risk of contrast-induced nephropathy (CIN).27 Irreversible deterioration in eGFR secondary to CIN, leading to progressive CKD, is associated with increased longer-term MACE, mediated through accelerated atherosclerosis, vascular calcification and effects on LV remodelling.27
European Society of Cardiology recommendations advocate renal optimisation through transient withholding of nephrotoxic medications, intravenous pre- and post-hydration, limited contrast use (lowest of either <350 ml or <4 ml/kg) and serum creatinine monitoring post procedure.28 LV end-diastolic pressure-guided fluid replacement in the POSEIDON study and the use of the RenalGuard (RenalGuard Solutions) system in the REMEDIAL II study both demonstrated a reduced risk of CIN compared with matched control cohorts.29,30 These strategies should be appropriately adopted to optimise both short- and longer-term renal outcomes, preventing irreversible progression of CKD, which itself begets SF. Further, with the advent of precision IVUS-guided PCI, the ability to safely perform complex intervention with minimal or zero contrast use has been demonstrated and is being incorporated into clinical practice.31
Dyslipidaemia
Dyslipidaemia is highly prevalent in the CTO population, at over 70% in the European Registry of CTO, and frequently coexists with diabetes and CKD.32 LDL, the target of statin therapy in preventive cardiovascular pharmacotherapeutics, has long been known as a risk factor for coronary artery disease.33 More recently, VLDL was found to be an independent predictor of ISR in people with diabetes after DES implantation.33 This was hypothesised to be mediated via the pathophysiological effects of apolipoproteins (Apo) B and C.34,35 However, HDL and ApoA1, the so-called ‘good cholesterol’, have been linked in vitro to improved stent biocompatibility through inhibition of smooth muscle cell proliferation, the suppression of inflammation and the prevention of neointimal hyperplasia.36
Furthermore, ApoA1 promotes re-endothelialisation following vessel trauma and stent implantation via generation of nitric oxide and facilitation of endothelial repair.36 This process is fundamental to stent strut coverage and hence prevention of ST. The REVEAL trial was the first to show an association between anacetrapib (a cholesterol ester transfer protein inhibitor)-driven increases in HDL and ApoA1 levels and a reduction in atherosclerotic vascular events, including cardiac death, MI and coronary revascularisation.37 Hence, rigorous management of cholesterol components, through lowering of LDL and VLDL while increasing HDL, appears important in halting aggressive atherosclerotic processes and optimising physiological stent biocompatibility.
Lesion-related Factors
Lesion length, location, composition and complexity are predictors of SF. Increasing CTO length predicts escalation through the hybrid algorithm and subsequent procedural success. In a retrospective analysis by Tian et al., 5-year outcomes demonstrated CTO length >15 mm to be a predictor of TLR, whereas Ahn et al. found CTO length >30 mm was associated with higher repeat PCI driven by TVR at 2 years.38,39 In the diabetic cohort of the OPEN-CTO study, approximately 60% had occlusion length >20 mm, whereas in the dissection and re-entry technique (DART) cohort of the CONSISTENT-CTO study, a mean (± SD) lesion length of 32 ± 22 mm was associated with an overall 2-year TVR of 14.9%, reiterating the potential for ISR and, further, development of downstream in-stent CTO.13,40
CTO location at the aorto-ostium or bifurcation increases procedural difficulty and carries a higher risk of SF. Aorto-ostial lesions are independent predictors of quantitative coronary angiography-based longitudinal stent deformation (LSD), and carry a higher chance of geographical miss, potentially leaving behind a nidus for TVR/TLR.41 The presence of a major bifurcation (within the proximal cap, occluded segment or distal cap) has been reported in 26–47% of CTO lesions and is associated with increased procedural complexity and longer-term MACE (primarily driven by reduced side-branch Thrombolysis in Myocardial Infarction [TIMI] flow and periprocedural MI).42 The strongest predictor of technical success where there is within-CTO side-branch involvement, is luminal side branch wiring at baseline, mitigating side branch loss, although this is not always feasible.42
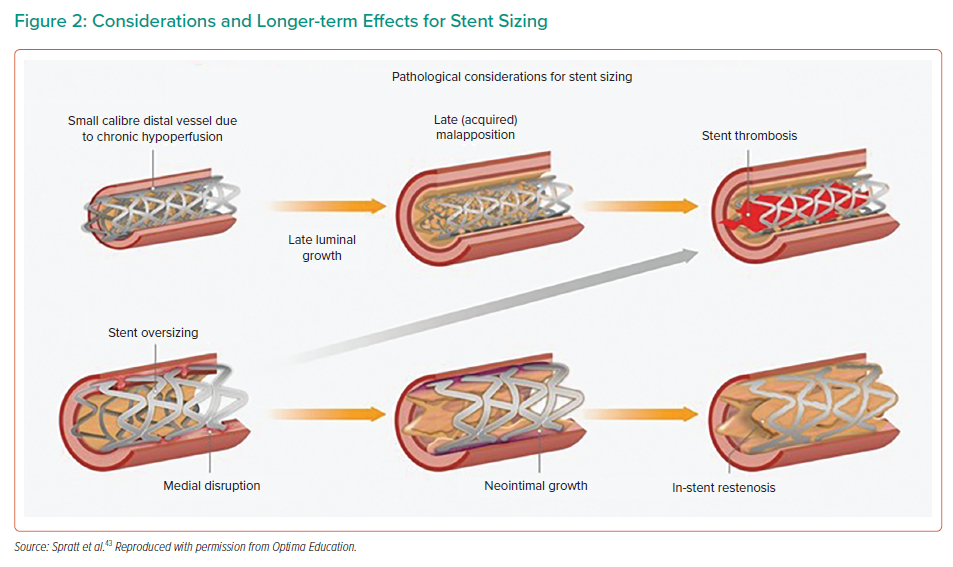
Lesion composition is dependent on CTO duration. Younger lesions display features of organised thrombus and necrotic core. Older lesions contain greater quantities of fibrous tissue and calcium, with a higher prevalence of negative remodelling.43 Heavily calcified lesions, particularly during the use of a subintimal (SI) strategy when aggressive modification carries an increased risk of perforation, are vulnerable to stent underexpansion or restriction, leading to an increased risk of both ISR and ST.43 Longer-duration CTO lesions without calcium often demonstrate significant negative remodelling, increasing the risk of vessel rupture with 1 : 1 stent sizing and leading to smaller minimum stent area (MSA), another independent predictor of ISR.43 Pathological considerations for stent sizing are shown in Figure 2.
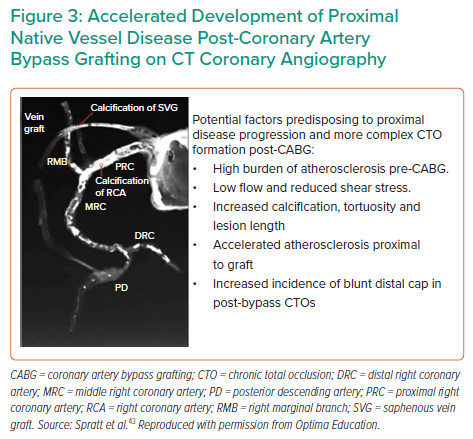
Post-CABG, CTO PCI adds an additional dimension of complexity to CTO recanalisation. Up to 40% of venous bypass grafts and 15% of internal mammary artery grafts occlude within 10 years.44 A study of native vessel patency after CABG demonstrated at least one new CTO in 43.6%.45 Pre-CABG native vessel stenosis >90% and Canadian Cardiovascular Society Class IV angina at baseline were independent predictors of subsequent postoperative CTO formation.45 Post-bypass CTO lesions exhibit increased calcification, negative remodelling and blunt proximal cap (Figure 3), rendering wire escalation strategies less successful (38%) than in non-CABG CTO (57%) and requiring early adoption of retrograde or DART strategies.46,47 Although TVR and MACE were higher in the post-CABG cohort, reassuringly 85% of patients remained event free at 1 year despite the complexity of their disease and procedural technique, alongside increased comorbidity.47
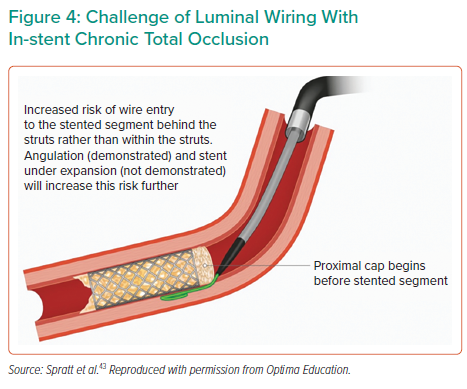
The in-stent (IS) CTO cohort poses further treatment complexity. Specific challenges include luminal wiring of previously under-expanded stents, with a higher likelihood of SI entry at the proximal cap (Figure 4) and increased calcification in these often longer-duration occlusions. Initial experiences of IS-CTO revascularisation reported success rates of 71%, whereas operator up-skilling and the use of novel devices have led to significant improvements, with an 86% success rate reported in both the PROGRESS-CTO registry and another large study by Azzalini et al.48,49 This is comparable to that of de novo CTO PCI, recognised to be around 90% when performed in high-volume centres by experienced CTO operators.13,48 Nevertheless, IS-CTO PCI carries a predilection to increased TLR and is independently associated with both increased MACE and repeat revascularisation.50
The prediction of CTO lesion complexity and procedural success through dedicated scoring systems is well established. Of these systems, the most commonly used J-CTO score has more recently been associated with trends in predicting 5-year TLR.51 In post-CABG CTO cohorts, the RECHARGE score (which includes a weighting for CABG) was deemed superior to the J-CTO score as an independent predictor of longer-term adverse outcomes, including TVF.52
Procedure-related Factors
Chronic Total Occlusion Recanalisation Strategy
Results of studies of the hybrid algorithm components (antegrade wire escalation, antegrade dissection and re-entry, retrograde wire escalation and retrograde dissection and re-entry) are mixed with regard to strategy-associated long-term TLR/TVR. An analysis of predictors of re-occlusion after DES supported CTO PCI in 802 successfully revascularised patients from the Florence CTO Registry, reporting a re-occlusion rate of 7.5%.53 The use of an SI tracking and re-entry (STAR) technique was associated with the highest re-occlusion rate (57%), compared with 5.1% in the non-STAR cohort.53 This was echoed in the J-PROCTOR 2 Study, where increased TVR was noted in a retrograde SI tracking cohort, and in a small meta-analysis of five studies where DART was associated with increased longer-term adverse events.54,55 However, the DART strategy itself is important, with use of newer device-based (CrossBoss and Stingray, Boston Scientific) approaches demonstrating significantly lower rates of MACE compared with older wire-based (STAR, limited antegrade subintimal tracking and controlled antegrade and retrograde tracking and dissection) techniques (8.9% versus 22.1%, respectively).56 Further, in regression analyses, wire-based DART and stent length were independent predictors of MACE.56,57 The use of DART in an earlier study by Rinfret et al. had a minimal impact on longer-term outcomes after CTO PCI and, most recently, SI stenting (48.1% of the cohort) in the CONSISTENT-CTO study neither adversely affected intravascular healing at 12 months nor was associated with higher TVR at 2 years.13,58 Differences between study outcomes, particularly those seen in CONSISTENT-CTO, may be explained by the higher rates (91%) of TIMI grade 3-defined procedural success and the adoption of pre-stenting IVUS (90.5% of cases).13 The results of the LOTUS ADR/RDR study, assessing long-term outcomes, including binary restenosis at the 13-month angiographic follow-up, 2-year TVR and validation of a dedicated restenosis score (R-Score) of related risk factors, are awaited.59
Intravascular Ultrasound
The use of IVUS in all PCIs has increased over the past decade. Global uptake and operator beliefs around the benefits of IVUS are highly variable by region.60 Although the British Cardiovascular Interventional Society’s national audit data show overall uptake at approximately 12%, a large study by Mentias et al. of more than 1 million Medicare patients in the US demonstrated an increase in IVUS use of only 3.9% (from 3% to 6.9%) between 2009 and 2017.61,62 However, another multicentre US registry reported a 38% frequency of IVUS.63 Hence, data are varied, perhaps (in the US) influenced to some extent by reimbursement. In contrast, in Japan, the country with the highest use of IVUS, registry data report >80% uptake.64 IVUS serves numerous roles, including: resolution of proximal cap ambiguity and guidance of cap penetration; facilitation of antegrade and retrograde DART techniques and prevention of dissection into the aorta; vessel and stent sizing; identification of appropriate landing zones, negative remodelling and calcium; and optimisation of stent expansion and apposition. IVUS also appropriately identifies nodular calcium and the extent to which the SI channel is in the adventitial space. This allows prediction of the risk of perforation with over-zealous post-dilatation, guiding the operator to accept a degree of eccentric stent expansion when appropriate and reasonable. The use of IVUS is associated with improved long-term outcomes in CTO PCI. Although the AVIO trial of angiography versus IVUS-guided PCI of complex lesions showed no significant difference in 2-year MACE, TLR or TVR, subgroup analysis revealed improved minimum lumen diameter (MLD) in the IVUS arm.65 However, CTO-specific analysis of IVUS versus angiography in the Korean-CTO registry found reductions in MACE, ST and TLR in longer (>30 mm) lesions in the AIR-CTO Study showed significantly lower rates of late lumen loss and ‘in-true-lumen’ stent restenosis and the CTO-IVUS Trial demonstrated reduction in MACE at 12 months.66–68 Hence, the use of IVUS, both up-front and for stent optimisation, can be deemed crucial in the prevention of longer-term SF and should be routinely used, regardless of CTO lesion complexity or recanalisation strategy.
Importantly, the demonstrated benefits of IVUS are reliant upon accurate image acquisition, interpretation and management of findings. RCTs of IVUS are prescriptive, protocolised to optimise results and often involve operators with greatest expertise, producing optimal outcomes. This is not reflective of real-world practice. Further, the importance of a final IVUS can be exemplified using rates of longitudinal stent deformation (LSD). In registry data, mean rates of approximately 1.2% are reported.41 However, the EXCEL substudy of stent deformation observed a 6.5% prevalence of LSD.69 This reiterates the importance of a final imaging run to systematically detect and correct anomalies predicting downstream SF such as LSD, tissue prolapse and edge dissection, in addition to ensuring good stent apposition and expansion.
Stenting Strategy
Stenting strategy, determined by stent platform, diameter, total stent length and post-deployment optimisation, is a key determinant of downstream SF. Evolution from BMS to DES witnessed significant reductions in ISR. This was mediated through reduced neointimal hyperplasia owing to DES bioactivity and reduced ST due to non-endothelialised stent struts, due, in part, to suppression of local inflammatory responses. A meta-analysis of 26,000 patients across 20 studies again supports the superiority of DES, with Picollo et al. demonstrating ST rates at 1- and 5-year follow-up after DES and BMS implantation of 0.6%, 1.1%, 8.4% and 13.4%, respectively, and corresponding TLR rates of 4% and 8.8%, 8.4% and 13.4%, respectively (p<0.001 for all).70 CTO-specific analysis of DES platforms in the FLORENCE-CTO Registry demonstrated superiority of EES over other DES, with significantly lower re-occlusion rates (3% versus 10.1%).53 However, other studies have found no significant differences between use of first- and second-generation DES, including Moreno et al., who demonstrated equipoise for restenosis between EES and sirolimus-eluting stent (SES) platforms following CTO PCI.71–73
Stent design, including strut thickness, radial strength and longitudinal integrity, affects the risk of LSD, StF and stent usability. Thinner strut designs that allow increased deliverability, trackability and vessel conformability are particularly advantageous in CTOs with tortuous and calcific anatomy or where coronary reconstruction with a ‘metal jacket’ of overlapping stents is required. Early studies of BMS, comparing thick (140 µm) and thin (50 µm) stent struts, found significant differences in both angiographic restenosis and TVR in favour of the thin strut design.74,75 This is supported by a recent network meta-analysis of 69 randomised controlled trials including over 80,000 patients, which demonstrated reductions in ST and MI with the use of ultrathin versus thick strut DES.76 The switch from stainless steel to cobalt chromium alloy in these thinner strut platforms allowed preservation of radial strength. However, clinical experience and data show a trade-off in longitudinal strength, rendering thinner strut designs more vulnerable to LSD.77
Although infrequent, with rates of 1.2% reported in the literature, LSD precipitates ST, TLF and MACE.41 Mechanisms relating to LSD are multifactorial, including, in addition to strut thickness, the number of connectors and their orientation. In bench testing, Ormiston et al. demonstrated that stent platforms with two connectors between hoops had reduced longitudinal strength on exposure to external forces compared with designs with six connectors, concluding that fewer connectors directly compromises longitudinal integrity.78 For example, the Promus Premier platform (Boston Scientific), a newer iteration of the two-connector Promus Element platform, saw the addition of extra connectors at the proximal stent end while maintaining a two-connector design through the main stent body, mitigating the occurrence of LSD while maintaining deliverability.79 This is an important consideration, particularly in the undertaking of aorto-ostial and bifurcation PCI.
StF, as a precipitant of SF, has been reported to occur at rates of 1–3% and is isolated to DES.80 Kuramitsu et al. studied StF of EES, finding increased MACE driven by ST and TLR (25.6% versus 2.3% in the non-StF group; p<0.001).80 Ostial stent location and lesions with hinge motion, tortuosity or increased calcium (prevalent in native and post-CABG CTOs) were independent predictors of StF.81 Platforms with increased radial strength serve to reduce the risk of StF in such lesions. In contrast to LSD, an increase in connectors confers greater risk of StF due to rigidity and reduced conformability to vessel anatomy and motion.79 An additional consideration in CTO PCI is the risk of stent undersizing due to negative remodelling, subintimal haematoma or poorer flow. Choosing a platform that can be appropriately overexpanded, particularly in long lesions or where there is distal and proximal vessel size mismatch, is important. This feature of the stent is primarily based on crown and connector design. The data demonstrate that with increasing overexpansion, crown straightening occurs.82 Although this can increase radial strength, it reduces flexibility and conformity, predisposing to StF. In addition, increased stent cell opening diameter can lead to intrastrut plaque prolapse and impair uniform drug elution, again risking SF.82 Balancing these factors when making stent choices during CTO PCI is key in longer-term procedural outcomes, and on-going development of the optimal stent platform continues as newer iterations manifest.
Stent length, akin to lesion length, alongside the number of stents deployed, predicts ISR. Ahn et al. studied outcomes after DES in long (>30 mm) versus short (<30 mm) CTO lesions.83 Although no significant differences in binary restenosis, late lumen loss or MLD were seen at the 6-month angiographic follow-up, higher repeat PCI driven by TVR was noted at 2 years.83 In the Korean CTO registry, lesion length >20 mm (p<0.01) and the use of at least three DES (p<0.001) were associated with MACE, TVR and TLR at a median follow-up of 22 months.84 Stent diameter and subsequent MSA are also strong predictors of SF. The combined TAXUS IV, V, VI and ATLAS Workhorse Trials’ IVUS substudy analysis of 1,580 patients demonstrated post-IVUS MSA >5.7 mm2 predicted 9-month angiographic stent patency.85 In smaller vessels, postintervention optical coherence tomography-assessed MSA <3.5 mm2 was found to be a predictor of 9-month ISR and TLR following PCI with a 2.5-mm diameter EES.86 IVUS analysis of MSA across different stent platforms (zotarolimus-eluting stent, EES and SES), revealed similar optimal MSA cut-off values for predicting ISR (5.2 mm2 and 5.4 mm2), with a smaller MSA predictive of angiographic ISR in first- and second-generation DES.87 In a CTO-specific study, Kang et al. found that the MLD and stent expansion ratio were independent predictors of ISR.88 These findings support the importance of image-guided PCI in CTO lesions to: allow accurate estimates of vessel sizing (and therefore stent diameter choice), particularly in the presence of vessel dissection or haematoma; rationalise maximal stent length; identify and appropriately modify calcium to facilitate stent expansion; and optimise stent expansion through post-dilation to achieve greatest MLD, MSA and stent expansion ratio in prevention of downstream ISR and ST.
Pharmacological Factors
Increased vessel trauma, the length of the stented segment and post-revascularisation vessel remodelling, alongside the often highly comorbid nature of this patient group, render the CTO PCI cohort at high risk for SF. RCT evidence over the past decade has led to paradigm shifts in dual antiplatelet regimes, with ticagrelor the preferred addition to aspirin for acute coronary syndrome presentations.89 In PCI for stable angina, Clopidogrel has remained the second agent of choice in addition to aspirin. Few studies specifically assess optimal platelet reactivity/responsivity or dual antiplatelet therapy choice after CTO PCI. The first analysis of platelet reactivity in a CTO cohort emerged from the FLORENCE CTO registry of more than 1,000 patients who underwent platelet function testing by light transmission aggregometry.90 The high platelet reactivity cohort had significantly increased cardiac mortality at 3 years compared with an optimal platelet reactivity cohort (p<0.001). Further, when those with high platelet reactivity were identified and clopidogrel (standard of care) switched to either prasugrel or ticagrelor, the survival rates seen were similar to those in the optimal platelet reactivity group.90 The TIGER trial, although small, demonstrated that ticagrelor pretreatment (compared with clopidogrel) improved downstream coronary vascular flow following CTO recanalisation, with the longer-term potential to improve ischaemia and reduce TLR.91 This is supported by data identifying TIMI flow grade as an independent predictor of TVF.92 Although larger RCTs to identify the optimal dual antiplatelet therapy strategy following CTO PCI are required and current guidelines offer no consensus, decisions will be at operator discretion and should factor in comprehensive assessment of patient-specific ischaemic and bleeding risk, alongside the complexity of CTO recanalisation, the extent of vessel stenting and final TIMI flow grade.
Conclusion
SF in both non-CTO and CTO PCI is multifactorial, involving patient comorbidities, cardiovascular risk factor control, lesion complexity, stenting strategy and, finally, antiplatelet and adjunctive medical therapy. As the prevalence of ischaemic risk factors continues to rise, preventive and therapeutic measures to mitigate these are paramount in the reduction of longer-term MACE and repeat revascularisation. Advances in interventional techniques, the development of novel devices and operator upskilling have led to the undertaking of PCI in increasingly complex and high-risk patient subsets. Specific to CTO PCI, increased calcification, the challenges of lesion preparation and stent optimisation in the SI space, where perforation risk is higher, and the potential for stent undersizing at the index procedure is greater, due to negative remodelling and haematoma increase the risk of SF. Therefore, it is crucial to optimise outcomes using a multipronged approach via aggressive medical therapy, lifestyle modification and meticulous image-guided precision PCI to reduce SF in these challenging patient cohorts.