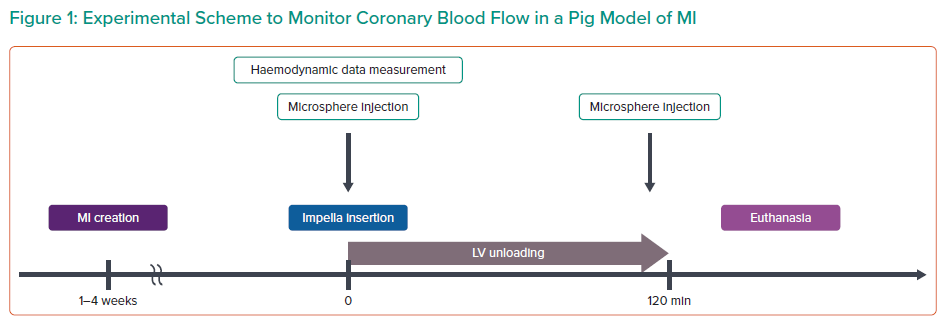
The goal of Dr Sakata’s work was to understand the effects of unloading on coronary blood flow. Previous work has shown that coronary flow is increased in the infarct zone with initiation of Impella, and this was correlated with end-diastolic wall stress.1 However, because increased coronary flow in the infarct area is highly variable, Dr Sakata and his team aimed to determine the factors that predict coronary flow improvement in the infarcted heart before and after Impella insertion using a porcine model. Briefly, 15 pigs underwent left ventricular (LV) unloading with Impella CP 1–4 weeks after MI (Figure 1). Fluorescent microspheres were injected prior to and after LV unloading to measure radial basis function (RBF), and linear regression analysis was conducted with baseline haemodynamic measurements to identify predictors of RBF improvement.
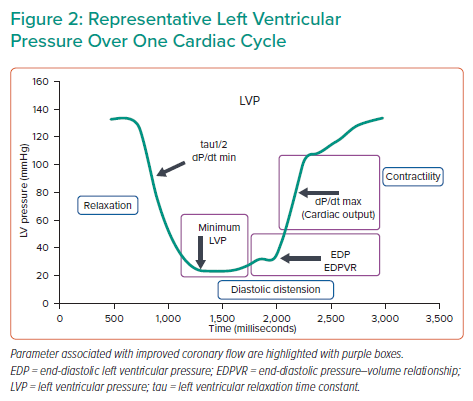
Coronary flow was measured before and after Impella support in the infarct, border and remote zones. Only coronary flow in the infarct zone showed a trend towards improvement under Impella support; however, statistical significance was not reached due to non-responders. Dr Sakata hypothesised that these non-responders were haemodynamically different from the animals with coronary flow improvements. Using univariate analysis, Dr Sakata showed that improvements in coronary flow were related to cardiac output, pulmonary arterial wedge pressure, left atrial pressure, minimum LV pressure (LVP), end-diastolic LV pressure, maximum dP/dt and the end-diastolic pressure–volume relationship (EDPVR). Multivariate analysis determined that maximum dP/dt and EDPVR were independent predictive factors of coronary flow improvement.
Ultimately, this study showed high EDVPR and low maximum dP/dt were associated with improved coronary flow under Impella support. High EDPVR was correlated with cardiac stiffness and low maximum dP/dt was correlated with decreased contractility, both commonly seen in patients after MI. This suggests that Impella may be more effective in improving coronary flow in ischaemic heart failure.
According to the present univariate analysis, factors that influence coronary flow span broadly over the cardiac cycle, from the beginning of LV filling to the isovolumic contraction phase (Figure 2). Dr Sakata’s next goal is to more precisely determine how coronary flow is increased. Ongoing studies aim to directly measure coronary flow simultaneously with LVP under unloading. Interestingly, preliminary results have shown that coronary flow is increased throughout all of diastole, consistent with the regression analysis results. Future work will focus on identifying the specific factors that cause these changes in each cardiac phase. Dr Sakata concluded that a higher EDPVR slope and lower maximum dP/dt are associated with better improvement in coronary blood flow in the infarct area during mechanical LV unloading.