Background
Left main (LM) coronary artery disease (CAD) represents an advanced stage of CAD, posing the risk of severe complications such as MI, heart failure and sudden cardiac death. About 5% of patients undergoing invasive coronary angiography receive a diagnosis of significant LM disease.1 The incidence of morbidity and mortality associated with LM CAD is notably elevated.2
There are many treatment options available for LM CAD, including medication, coronary artery bypass graft (CABG) surgery and percutaneous coronary intervention (PCI). Traditionally, CABG has served as the primary revascularisation method for LM CAD. However, the past decade has witnessed noteworthy progress in PCI techniques and equipment, expanding the role of PCI in LM revascularisation and the use of PCI for LM CAD has established itself as a viable alternative to CABG for selected patients and comparable long-term rates of major adverse outcomes have been documented.3,4,5 According to the 2009 American Heart Association guideline, PCI for LM lesions holds a class IIb recommendation.6 The latest European guidelines recommend PCI for LM CAD based on SYNTAX score, with a class I recommendation for patients with low SYNTAX scores, class IIa for those with intermediate scores and class III for individuals with high SYNTAX scores.7
An evidence gap exists regarding the clinical outcomes of PCI for LM CAD in Vietnam. This research aims to address this problem by presenting our experiences of PCI for LM CAD at a tertiary healthcare centre in Ho Chi Minh City, Vietnam. The primary objective is to assess the outcomes of PCI, encompassing in-hospital and post-discharge mortality rates. A secondary objective is to document the outcomes of patients undergoing LM PCI over a 1-year follow-up period and to evaluate the concordance of these outcomes with studies conducted at other institutions worldwide. Our intention is to provide an alternative perspective regarding the practice of LM coronary intervention in Vietnam, a developing country faced with limitations in adopting up-to-date techniques due to various constraints.
Methods
This prospective observational study has been approved by Nguyen Tri Phuong Hospital’s Ethical Review Committee and follows the principles outlined in the Helsinki Declaration. The study was conducted from July 2015 to July 2023 at Nguyen Tri Phuong Hospital, Vietnam. Informed consent was obtained from patients or their first-degree relatives.
Study Population
We included all adults hospitalised with LM CAD who underwent PCI. Individuals under 18 years of age, those with conditions hindering LM coronary intervention, those who declined participation and those with a history of CABG were excluded from the study. Patients were diagnosed with either chronic or acute coronary syndrome, encompassing acute ST and non-ST segment elevation MI (STEMI and NSTEMI) and unstable angina (UA). Significant LM disease was determined based on a visual assessment of stenosis diameter ≥50%.
Pre-procedural patient data were collected, including information on comorbidities and risk factors such as smoking, diabetes, hypertension, dyslipidaemia, chronic kidney disease, family history of cardiovascular disease and BMI measurement. Laboratory data, including troponin I, glycated haemoglobin (HbA1c) and serum LDL levels, were also collected. ECG and echocardiography were performed to estimate the left ventricular ejection fraction.
In our study, intracoronary imaging, such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT), was not performed due to high costs and limited availability in Vietnam.
Catheterisation Procedure
The choices of access site, intervention technique and stent technique were based on the operator’s decision, adhering to the recommendations of the European Bifurcation Club. The specific steps varied depending on the selected technique.
During the procedure, IV unfractionated heparin was administered. All patients received acetylsalicylic acid (aspirin) and a P2Y12 inhibitor (clopidogrel or ticagrelor). The angiographic study comprised SYNTAX score evaluation and Thrombolysis in MI (TIMI) flow grading. The CABG team were consulted about patients with high SYNTAX scores and they were given detailed counseling regarding the indications favouring CABG over PCI. The decision to conduct PCI was made due to increased surgical risks, ineligibility for surgical procedures or when a patient refused to undergo CABG. Patients who chose PCI were made aware of the risks and provided informed consent before they were included in the study.
Coronary guidewires were introduced into the left anterior descending (LAD) and circumflex (LCx) arteries. One of these arteries – either the LAD or LCx – was designated as the main branch, while the other served as the side branch. Lesion preparation was conducted before stenting the LAD, with a wire inserted into the side branch to maintain blood flow and access to the side vessel. After stenting from the LM artery into the main branch, the proximal optimisation technique (POT) would be performed if necessary. Kissing balloon inflations could also be carried out, followed by additional POT (Supplementary Figure 1). The choice of stent in our study was left for the operator to decide. Only second-generation drug-eluting stents (DES) were used, including stent systems containing paclitaxel, sirolimus, and everolimus.
Technical success was defined as the completion of stent placement, balloon dilation, rewiring, and final kissing balloon therapy, as required by the protocol. It also involved the successful placement of stents with TIMI 3 flow and less than 30% stenosis in any stented vessel, as well as TIMI 3 flow in any unstented vessel. Clinical success was defined as the achievement of technical success, with no adverse in-hospital outcomes documented (including death, MI and emergency CABG).
Post-procedure
After the procedure, all patients received optimal medical therapy in accordance with the current European treatment guidelines.7 This regimen involved a sustained daily intake of aspirin 75–100 mg and a P2Y12 inhibitor (either clopidogrel or ticagrelor) for up to 1-year post-operatively. Statin therapy – rosuvastatin or atorvastatin – was consistently maintained throughout the study.
Follow-up
After undergoing PCI, patients were transferred to the post-PCI division of the cardiovascular intervention department and subsequently discharged if they maintained stability for 24 hours. Post-discharge, all patients were followed up as outpatients in our department. In accordance with hospital protocol, follow-up visits were scheduled at 7 days and 30 days post-discharge, with subsequent monthly appointments.
Outcome Definition
The primary outcome was the incidence of major adverse cardiac and cerebral events (MACCE) and target vessel failure (TVF). MACCE was defined as cardiovascular mortality, non-fatal MI, non-fatal cerebrovascular events and acute coronary syndrome that required hospitalisation. TVF is defined as the composite of cardiac death, target lesion MI and any target vessel revascularisation.
The secondary outcome was contrast-induced nephropathy (CIN) which was defined as an elevation of serum creatinine of more than 25% or ≥0.5 mg/dl (44 μmol/l) from baseline within 48 hours after the catheterisation procedure. Other procedural complications, such as haemorrhage or haematoma, were also assessed.
Patient Classification
The universal definition of MI was employed to identify patients with acute coronary syndrome (ACS) or chronic coronary syndrome (CCS).8
Statistical Analysis
Data were analysed using the statistical and data software (Stata 17). Quantitative data were presented as mean ± standard deviation (SD) for normally distributed variables or as median (interquartile range [IQR]) for non-normally distributed ones. Qualitative variables were represented as frequencies. The X2 test or Fisher’s exact test was used to analyse differences for qualitative variables, while quantitative variables underwent analysis of variance (ANOVA) or the Kruskal–Wallis H-test. Univariate and multiple linear regression analyses were performed to identify factors relating to adverse outcomes. R statistical significance was defined as p≤0.05.
Results
Between July 2015 and July 2023, 63 patients with LM CAD were diagnosed at our hospital. However, among these, two patients died upon admission before any intervention could be administered. Additionally, one patient declined all forms of treatment and another was transferred to the Ho Chi Minh Heart Institute for further care. So in total we enrolled 59 patients who underwent PCI for LM lesions. A detailed flow chart of the study is provided in Supplementary Figure 2.
The patients were divided into two groups based on their diagnosis: ACS or CCS. The primary endpoints were monitored at three different time points: during the patient’s hospital stay, 30 days after the procedure and 1-year post-procedure. The characteristics and clinical features of the patients were analysed (Supplementary Table 1). The average age of the patients was 66.7 ± 1.5 years. At the time of presentation, 10 patients (16.9%) were diagnosed with CCS and 49 (84.1%) were diagnosed with ACS. Over the follow-up period, 11 cases of death (18.6%) were confirmed. The mortality rate during the hospital stay was 5.1% (n=3), which increased to 11.9% (n=7) after 1-year follow-up. The average hospitalisation period was 12.4 ± 1.3 days.
The average haemoglobin concentration in the study was 121.2 ± 24.8 g/dl. Most patients were not anaemic at admission and the median estimated glomerular filtration rate was 63 ml/min (59–77). The prevalence of lipid disorders was high, accounting for 55.9% of the study population, with an LDL concentration of 2.8 (2.4–3.2) mmol/l and an average HbA1c of 6.8 ± 1.8. This result indicates that a relatively large proportion of the patients had metabolic disorders. Most patients (69.5%) had a normal ejection fraction (EF) and more than 90% had sinus rhythm on ECG, while 62% had ST-T elevation at admission (Supplementary Table 2)
The average SYNTAX scores were 30.2 ± 3.0 for the CCS group and 29.2 ± 1.1 for the ACS group (p=0.7). Over 50% of patients in the CCS and ACS groups had triple-vessel coronary disease (p=0.5). The distribution of bifurcation was primarily LM-LAD-LCX in patients in both groups, with the most common Medina classification being 1,1,1 (50% in each group, p=0.3). Kissing balloons were conducted in 30% of cases in the CCS group and 50% in the ACS group (p=0.2). In both groups, all patients exhibited TIMI III flow after. Final post-dilation optimisation was performed in 10% of CCS cases and 35% of ACS cases (p=0.1). Regarding additional vessel stenting, interventions in the LAD was predominant in both groups (40% and 42.9% in the CCS and ACS respectively, p=0.8). Two cases in the ACS group had coronary dissection during the procedure; however, these complications were successfully managed by additional stent implementation (Supplementary Table 3).
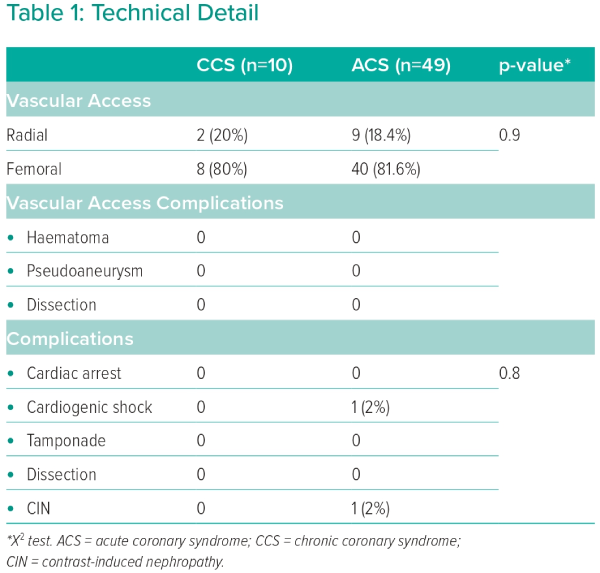
Femoral access was the primary method used for both groups and no vascular access complications were observed. Only two cases with major complications were recorded. One patient was diagnosed with cardiogenic shock and the other was diagnosed with contrast-induced nephropathy (CIN). Both of these cases were in the ACS group (Table 1).
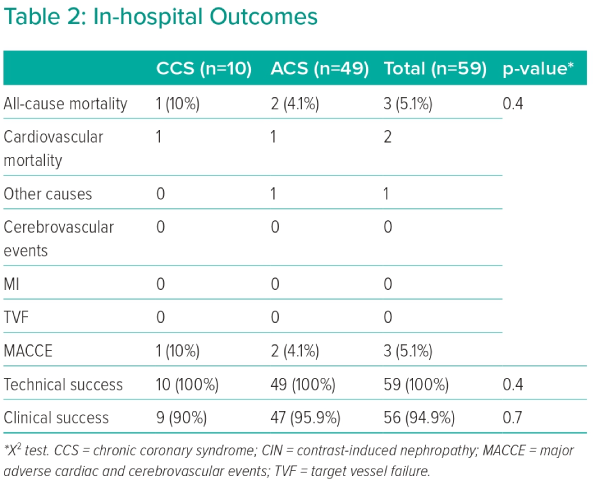
There were no statistically significant differences in in-hospital outcomes between the two groups. One patient in the CCS group and two in the ACS group died in hospital. In the ACS group, one death resulted from acute heart failure and one from acute kidney injury due to CIN. The mortality case in the CCS group was due to acute heart failure. This led to the overall MACCE rate during the hospital stay, which was 4.1% for patients with ACS and 10% for the CCS group. Technical success was achieved in all patients in both groups. However, the clinical success rate was 90% in the CCS group and 95.9% in the ACS group (Table 2).
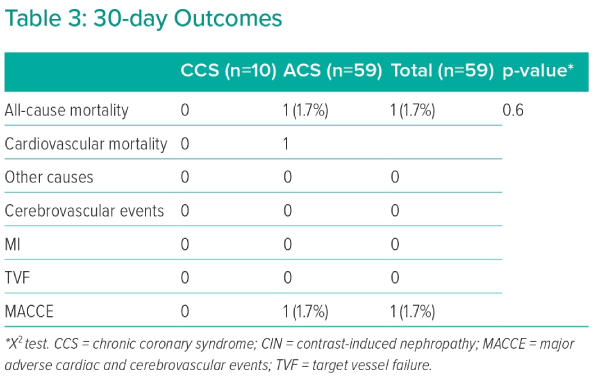
The 30-day all-cause mortality rate in the ACS group was 2.1%. Among the cases in this group, there was a single instance of cardiovascular death, contributing to the overall rate of MACCE at 30 days, which was also 2.1% in the ACS group (Table 3).
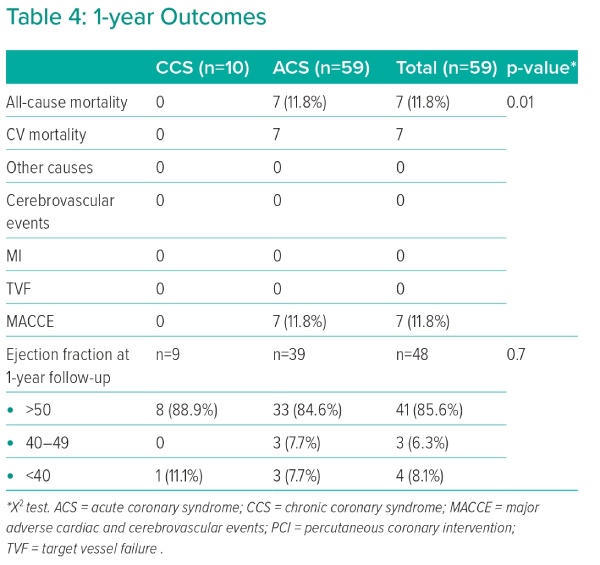
The overall rate of MACCE was mainly driven by cardiovascular deaths, which occurred in seven out of 46 patients (15.2%) in the ACS group. All cases resulted from acute heart failure. After a 1-year follow-up, EF remained over 50% predominantly in both groups. Only 11.1% of patients in the CCS group and 7.7% in the ACS group exhibited a reduced EF (Table 4).
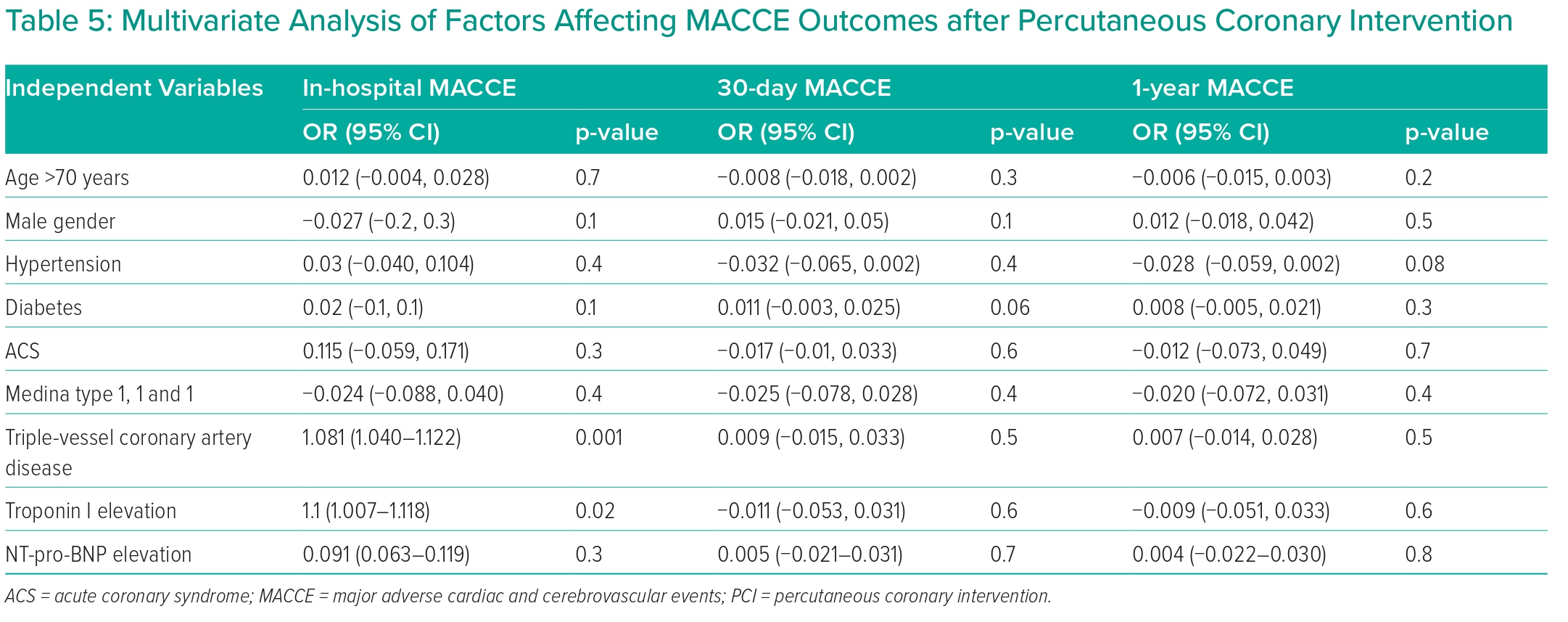
Based on multivariate regression analysis, triple-vessel CAD and a high troponin I level were significant independent predictors of in-hospital MACCE in patients with LM disease (OR 1.081; 95% CI [1.040–1.122], p=0.001) and (OR 1.1; 95% CI [1.007–1.118], p=0.02), respectively. No other relationships were observed between other factors and MACCE outcomes at 1-month and 12-month intervals. These findings suggest the predictive value of specific coronary conditions and troponin I levels in the context of in-hospital MACCE occurrences (Table 5).
Discussion
CABG is considered the preferred treatment for LM CAD. However, recent evidence shows that PCI is non-inferior to CABG for treating LM CAD.5 In our study, the accumulated incidence of MACCE at the 1-year follow-up was 18.6%, which is marginally higher compared to other major trials. The EXCEL trial reported that within its PCI group, the incidence of major adverse events at 30 days was 4.9%. However, this figure rose to 15.4% after 3 years and further increased to 22% over the 5-year follow-up.9 Additionally, the NOBEL trial recorded a 30-day MACCE rate of 2.5% post-PCI, which subsequently escalated to 28.9% after 5 years.10 The 10-year results from the PRECOMBAT trial showed that MACCE and all-cause mortality in PCI groups reached 18.2% (Supplementary Table 4).11 However, it is important to note that these trials were conducted under stringent conditions in healthcare systems known for their advanced levels of care, both pre- and post-intervention. Another contributing factor to their outcomes may be the widespread use of advanced intracoronary imaging in these trials, a practice not commonly seen in developing countries. In the study by Kumar et al. in India, the in-hospital MACCE rate was 1.8%, which increased to 11.5% over a 2-year follow-up period. It is noteworthy that intracoronary imaging was used in only 23.6% of LM interventions in this study.12 Similarly, the study by Ayman et al. in Egypt revealed that IVUS or fractional flow reserve (FFR) techniques were used in merely 6.34% of LM intervention cases. Consequently, this resulted in a MACCE rate exceeding 20% at the 1-year follow-up, regardless of the intervention methods used.13 Despite the proven benefits of intravascular imaging, its widespread adoption in developing countries is hindered by many factors such as high costs, limited availability and insufficient training. In Vietnam, significant efforts are being made to address these challenges and to promote the broader use of intravascular imaging techniques in medical practice.
At the 30-day follow-up, our study did not find any statistically significant differences between the ACS and CCS groups in terms of MACCE. However, our study did identify a higher mortality rate after 1 year in the ACS group compared to the CCS group, despite the same clinical and demographic characteristics between the two groups. This indicates that the risk for ACS patients remains elevated even with aggressive therapy.14
Furthermore, our study revealed no significant difference in the outcomes of the PCI technique between ACS patients and those with CCS. Both groups exhibited a favourable final angiographic result and no vascular access complications were observed. Although only two patients experienced major complications, these were confined to the ACS group. Notably, no cases of stent thrombosis were confirmed. The relatively low incidence of stent thrombosis provides reassurance. It can be attributed to using thinner-strut second and third-generation stents and the improvement of optimal implantation techniques for LM lesion.15
Our research also found that patients with three-vessel coronary artery lesions or elevated troponin I levels had higher intra-hospital events. This result, aligned with other studies, indicates that in patients undergoing PCI for LM CAD, those admitted for ACS would have poorer outcomes. Jia et al. demonstrated that patients admitted with STEMI and concurrent LM disease had higher risks of all-cause mortality within a 2-year period (12.5 versus 3.0%, p=0.013), cardiac death (12.5% versus 1.3%, p=0.005), MI (16.7% versus 2.2%, p=0.002) and stent thrombosis (12.5% versus 1.0%, p=0.002) compared to those without LM CAD. Similarly, patients admitted with UA/NSTEMI and LM involvement exhibited higher rates of MI (5.3% versus 1.8%, p=0.010), stent thrombosis (3.1% versus 0.8%, p=0.022) and stroke (4.6% versus 1.5%, p=0.016) compared to patients without LM disease.16 These findings imply that the concurrence of ACS and LM disease is predisposed to heightened risk, particularly in cases where the culprit lesion involves the LM coronary artery. The extensive perfusion territory of the LM, irrespective of coronary artery anatomical dominance, underscores the prognostic significance of acute LM injury and concurrent multivessel coronary artery involvement in infarction events, which could lead to large infarct zones and unfavourable clinical outcomes.17,18
In summary, our findings suggest that PCI for LM CAD can be considered a relatively safe alternative to CABG, demonstrating acceptable rates of adverse events, particularly in centres where resources for CABG surgery and intracoronary imaging are constrained.
Study Limitations
The study was not without limitations. These included a relatively small sample size and a follow-up period of just 1 year. Additionally, the assessment of lesions in the LM artery and the guidance of procedures using adjunctive techniques such as IVUS, FFR or OCT were constrained due to the resources available at our hospital.
Conclusion
While CABG remains the standard treatment for LM coronary lesions, PCI could be considered an alternative for patients requiring revascularisation when CABG is not preferred. Factors such as three-vessel CAD and elevated troponin I levels could be clinical predictors of in-hospital adverse outcomes in patients with LM disease.19 
Click here to view Supplementary Material
Clinical Perspective
- Percutaneous coronary intervention could be considered an alternative to coronary artery bypass surgery to treat left main coronary artery disease with favourable outcomes both in hospital and in the mid-term.
- In developing countries, where there may be constraints on the availability of advanced intracoronary imaging techniques and resources for coronary artery bypass surgery, percutaneous coronary intervention for left main artery disease can yield successful results, provided that there is meticulous selection of patients and the procedures are performed by experienced operators.
- It is critical to integrate advanced intracoronary imaging techniques into the treatment protocol whenever feasible.