Coronary CTA has rapidly gone from a test with potential to be considered a first-line test for patients with stable chest pain.1 It provides robust ability to exclude atherosclerosis and coronary artery stenosis and more recently has been shown to inform and guide clinical treatment making in a fashion that enables a reduction in myocardial infarction when compared to traditional stress testing.2–5 Despite the growing clinical utility data and continued technology improvements, resulting in improved image quality with lower radiation exposure, coronary CTA remains an anatomical test which cannot provide the necessary adjudication of ischaemia needed to guide revascularisation.6 As well, while very robust at ruling out stenosis, the specificity of coronary CTA is limited by spatial resolution, particularly in the setting of significant calcification, which will be a growing issue with CCTA now considered an appropriate first-line test in patients with higher pre-test likelihood of CAD.6
To help manage both of these limitations we have seen the development of both CT perfusion and non-invasive fractional flow reserve (FFRCT) derived from CT. FFRCT was first introduced in 2010 and has undergone significant maturation and validation. The version used clinically, and extensively validated, employs computational fluid dynamics to solve the equations that govern flow and resistance in the coronary arteries while computationally simulating hyperaemia, thereby obviating the need for adenosine administration.7–10 This test is also appealing as it does not require a change in CTA protocols and does not require additional radiation exposure. Through the validation of the technology, FFRCT has been proven to significantly improve the specificity of CTA for the discrimination of ischaemia as defined by invasive FFR. In the most recent large-scale multicentre trial, FFRCT accurately reclassified 68 % of CTA false positives to true negatives without a compromise in sensitivity.7
Much of the early clinical trial work and clinical focus has been placed on the avoidance of invasive angiography in patients with anatomical stenoses on CTA. While a meaningful opportunity to help overcome a limitation of clinical CT adoption, it is not the only role for FFRCT in stable chest pain. This is particularly the case as CCTA is being used in patients with higher pre-test likelihood, more coronary calcification and more complicated coronary artery disease (CAD).10 In these patients, FFRCT has been shown to be effective in characterising lesion specific ischaemia despite the higher burden of coronary artery calcium (CACS). Norgaard and colleagues,11 in a sub-analysis of the NXT trial evaluated the diagnostic performance of FFRCT in the setting of higher CACS and noted that while the diagnostic accuracy of FFRCT was slightly lower at CACS >400 it was not significantly so, unlike CCTA alone, the accuracy of which was significantly worsened.
Moving Beyond ICA Deferral
Beyond diagnosis and risk stratification, the role of non-invasive imaging has always been to help enrich the population referred to the catheterisation laboratory. It has become increasingly clear that traditional stress testing is not effective in discrimination of those who are likely to be found to have actionable coronary artery disease. Given the apparent disconnect between stress testing and findings at the time of invasive coronary angiography (ICA) and the lack of anatomical information provided by stress testing, there has been little integration of non-invasive imaging in the guidance of revascularisation decision-making at the time of ICA. With the maturation of CCTA and the integration of FFRCT there is the opportunity to not only rule out disease with CCTA but to help guide and plan ICA and revascularisation strategies on the basis of anatomical stenosis and lesion specific ischaemia. Jensen and colleagues recently confirmed a significant increase in the percutaneous coronary intervention (PCI)/ICA ratio particularly in the higher risk population, importantly with PCI adjudicated by invasive physiology as well.12 In addition, ICA was cancelled more frequently in the high risk population on the basis of FFRCT (75 %) versus CTA alone (45 %). These data introduce the possibility of PCI decision-making without needing to adjudicate ischaemia invasively owing to the high concordance between non-invasive and invasive measures of ischaemia. Given the growing evidence of the relatively high frequency of and the increased hazard associated with incomplete revascularisation, the need to develop a more thoughtful approach to revascularisation seems necessary.
With this growing and clear need, investigators have begun to explore ways of using non-invasive imaging data to help inform interventional strategies. Collet and colleagues also recently evaluated the potential that a non-invasive approach to adjudication of anatomy and physiology could act as a surrogate in treatment decision-making for invasive evaluation in the SYNTAX II trial (SYNTAX II). Interestingly, the authors found that there was poor correlation between the invasive and non-invasive anatomical syntax but much better correlation between the non-invasive and invasive functional syntax score.13 The anatomical SYNTAX score was overestimated by CTA compared with conventional angiography (27.6 ± 6.4 versus 25.3 ± 6.9; p<0.0001) whereas the calculation of the functional SYNTAX score yielded similar results between the non-invasive and invasive imaging modalities (21.6 ± 7.8 versus 21.2 ± 8.8; p=0.589) (Figure 1). In fact, in patients with three-vessel disease the CTA SYNTAX score almost uniformly overestimates the anatomical SYNTAX score derived from coronary angiography whereas the non-invasive functional SYNTAX score (FSS) was both feasible and yielded similar FSS compared to the invasive FSS and allowed similar reclassification rates. Being able to provide a non-invasive FSS offers significant potential to reduce resource utilisation at the time of ICA through reducing the need for invasive adjudication of ischaemia and by enabling the development of a revascularisation strategy in advance of ICA. In addition, by providing a non-biased three-vessel anatomical and physiological mode, the historical anatomical bias that determined whether ischaemia should be adjudicated no longer exist. Given the growing evidence that incomplete ischaemic revascularisation results in worsened event-free survival, tools that allow for effective decision-making that results in a higher likelihood of full ischaemic revascularisation should be considered.
This premise has been tested in the SYNTAX III trial which just recently completed enrolling. In this trial, subjects were randomised to non-invasive and invasive physiological adjudication of ischaemia. The results were reported at EuroPCR 2018 with the findings highlighting strong good agreement of treatment decision-making between CTA/ FFRCT and ICA/FFR strategy (Cohen’s kappa=0.82; CI: 0.73–0.91). The heart teams agreed on the coronary segments to be revascularised in 81.1 % of the cases. As well, FFRCT changed the treatment decision in 7 % (14/196) of the patients with 13 patients having a recommendation of surgical revascularisation changed to a percutaneous approach. Importantly, in both of these studies, CTA/FFRCT did not define the treatment but did provide important proof of concept and data to enable the initiation of the SYNTAX IV trial where patients will be randomly assigned to treatment decision-making by CTA/FFRCT versus the traditional approach of ICA/FFR. This trial represents the next step towards meaningfully embedding non-invasive imaging in interventional and revascularisation planning.

Reinvigoration of the Heart Team
Over the last 15 years, we have seen a reinvigoration of the Heart team in the context of transcatheter aortic valve replacement (TAVR). This Heart team strategy has been pivotal in helping TAVR with its rapid evolution and clinical adoption. This collaborative pre-procedural discussion has allowed more informed and collaborative decision-making. These discussions have also allowed for deeper integration of non-invasive imaging in the structural space by allowing the imager to better understand the clinical needs and the interventionalists to better understand how non-invasive imaging can help inform decision-making and improve clinical outcomes. Unfortunately, the evolution of percutaneous coronary intervention has largely happened in isolation at least in part owing to the historical lack of meaningful non-invasive imaging to support decision-making. While invasive angiography is the gold standard for anatomy, with the improvements in coronary CTA and now advanced computational analytics offering non-invasive FFR, delta FFRCT, plaque and coronary geometry, it is time to revisit the coronary heart team for coronary artery disease. Perhaps the days of going to the catheterisation laboratory on the basis of symptoms and a nuclear stress test without any knowledge as to the extent, severity, or pattern of CAD are numbered. It would be hard to imagine going to the hybrid surgical suite and performing a TAVR without any baseline imaging or sizing of the annulus nor an assessment of anatomical drivers of procedural complications in the same way surgeons would not go to the operating room without imaging to provide an initial plan. Clearly, the incremental value of CTA FFRCT will need to be proven in a prospective randomised fashion but the opportunity is finally a reality.
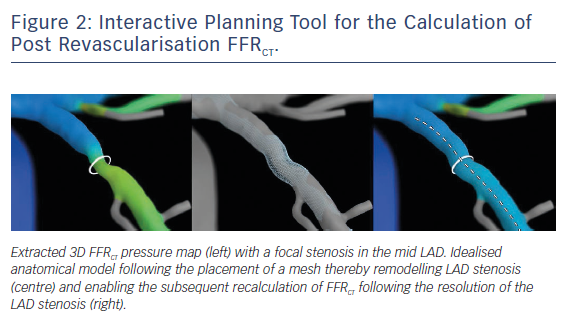
Recently, the concept of an interventional planner has been introduced where an idealised model is created to simulate the post PCI coronary artery allowing the calculation of a post-PCI FFRCT (Figure 2).14 This pre-procedural calculation of post procedural physiology offers another opportunity to help further guide the interventionalist with revascularisation decision-making. In the original feasibility accuracy study, virtual post FFRCT displayed fairly robust diagnostic performance for the prediction of post-PCI physiology. This initial version was limited in scope and clinical utility owing to the computational requirements which could not be met to allow timely enough modelling to be used for clinical care. With further improvements in computational capacity these idealised models can now be performed by physicians at their site, thereby opening up the opportunity to help inform revascularisation decision-making. Clearly this interactive planner will need further diagnostic performance validation and then ultimately, if proven to be robust, to determine its clinical utility and impact on clinical decision-making and downstream clinical outcomes.
Challenges
There remain challenges with the integration of FFRCT into the clinical paradigm. The technological hurdles regarding computational processing have been significantly reducted in the turnaround time from 24 hours at the time of initial release to <5 hours in the large majority of cases at present. Lack of reimbursement in some healthcare environments has also posed meaningful challenges towards broad adoption. These economic and funding issues will need to continue to be managed globally to see meaningful pervasion into clinical practice. Finally, non-invasive diagnosis of coronary artery disease has long been dependent on ischaemia testing, this established practice pattern has supported the field for decades and shifting practice is not a minor task. It is possible that the demand from an interventional perspective for a roadmap prior to invasive evaluation may impact initial test selection amongst symptomatic patients with suspected CAD.
The Way Forward
To tackle a disease as complex as CAD, having more information prior to the intervention may help with thoughtful and controlled decision-making. Recently, there has been increasing evidence of the incidence and associated risk of incomplete ischaemic revascularisation. Choi and colleagues found that approximately 25 % of patients undergoing multivessel disease revascularisation do not experience complete ischaemic revascularisation. Importantly, these subjects had a significantly higher MACE rate in multivariate analysis (adjusted hazard ratio: 4.17; 95 % confidence interval: 1.85–9.44; p<0.001).15 Whether pre-procedural review of CT anatomical and physiological findings will translate to more complete and appropriate revascularisation has yet to be proven but if so could result in a significant shift in the management of CAD. This hypothesis needs to be tested in a trial setting. SYNTAX IV will help fill the data gap but additional data are required from populations referred for invasive angiography.
While it remains early in the clinical adoption of FFRCT and other advanced computational analytics in clinical practice with many outstanding clinical questions, we may be witnessing a paradigm shift in the management of coronary artery disease. It is possible that in the not-so-distant future that the majority of patients will go to the catheterisation laboratory with an interventional strategy in mind with a large majority undergoing ICA and also undergoing PCI. Beyond simply improving catheterisation laboratory efficiency, the ultimate goal is to ensure that those that undergo PCI receive the intended benefit of complete ischaemic revascularisation which the current paradigm is not offering with a high enough frequency.