An Introduction to Radiation
X-rays, so-called because their nature was at the time unknown, were discovered by the German physicist Wilhelm Roentgen in 1895, one year before the discovery of ‘natural’ radioactivity by Henri Becquerel.1
X-rays found application in radiography a few years after their discovery, although the first side effect attributed to radiation injury (depilation) had been described prior to this – in March 1896.
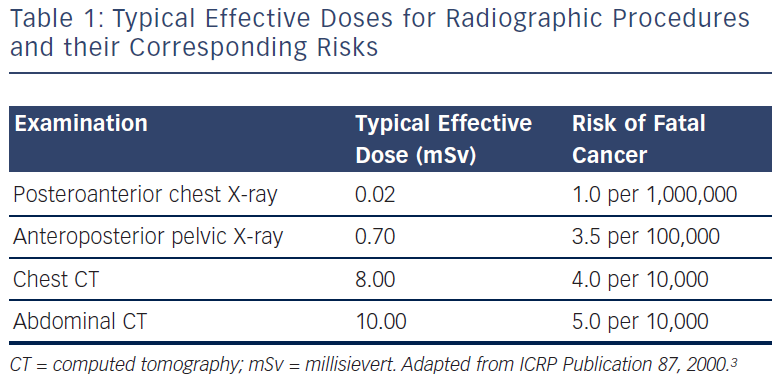
X-ray imaging subsequently developed into an important medical technique. It was estimated that more than two billion X-ray examinations were performed in the US in 20082 and that medical uses represent the largest source of radiation exposure to the US population.3 However, although X-ray imaging has great medical benefits, it poses an important risk for patients and healthcare staff, which is reviewed in this article.
The International Commission on Radiological Protection (ICRP) recommends the use of the ‘effective dose (ED)’ measure to evaluate the effects of partial exposure and equate the associated risks to those of whole-body exposure.
- Radiation dose = (radiation energy absorbed by patient) / (mass of tissue irradiated).
- Unit: 1 gray (Gy) = 1 joule per kilogram (J/kg).
- ED = absorbed dose corrected for radiation type (e.g. X-ray) and tissue type weighting factors.
- Unit: 1 sievert (Sv) = 1 Gy to the whole body.
Biological Effects of Radiation
The effects of ionising radiation on health are classified broadly as either deterministic or stochastic. Exposure to high levels of radiation causes tissue damage as a consequence of the killing or gross malfunction of cells. These ‘deterministic’ effects only occur above a given dose threshold and exhibit steeply increasing severity with increasing dose above this threshold. Examples of deterministic effects of radiation are skin injury and the formation of cataracts.5
Conversely, stochastic effects of radiation can occur at any dose level (rather than above a threshold), exhibiting an increasing probability of the effect proportionate to the exposure level. Typical stochastic effects are the mutation of cells following DNA damage or the development of a malignancy.6,7 No proof exists of stochastic effects at doses less than 100 millisievert (mSv); however, the ICRP recommends a linear, no-threshold regression model to evaluate risk in this dose range.8
The ICRP quantifies the relationship between ED and the probability of developing lethal cancer as approximately 5 % per 1 Sv of exposure.7 Thus for a population receiving a 0.2 Sv dose, this translates to 1 % of individuals who may in the long term develop lethal cancer as a consequence of exposure. For a typical cardiac examination administering a lower dose, an ED of 10 mSv, the risk of cancer has been estimated at 1 in 2,000.7 The ICRP recommends an annual limit of 20 mSv/year for occupational exposure and 1 mSv/year for the public.7
Radiation in the Catheterisation Laboratory
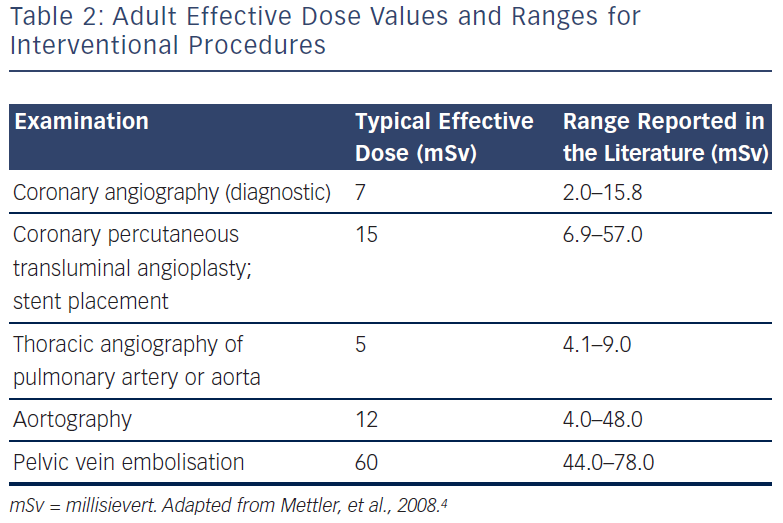
The cath lab is an environment in which the working staff (cardiologists, radiographers, technicians, nurses and trainees) risk radiation exposure on almost a daily basis, and achieving adequate protection for staff during procedures remains problematic. Staff exposure to radiation in the cardiac cath lab is generally considered to be higher than in other therapeutic laboratories that use X-ray equipment (radiology, urology, operating rooms) because the staff work in close proximity to the patient. In addition, factors including the configuration of the X-ray equipment, the distance to the X-ray source, the number of cases performed per day, and the often long period of screening required for a procedure can all contribute to this relatively high level of exposure. The radiation dose measures for staff members in the cath lab who wear dosimeter badges both inside and outside their lead aprons are generally among the highest in the hospital.
There are two different sequences of radiation exposure in the cath lab – fluoroscopy and acquisition (cine). Fluoroscopy is used for catheter, balloon and stent placement, and involves 50–90 % of the total X-ray operation time. However, fluoroscopy only accounts for approximately 20 % of the total radiation exposure to staff and patients. Acquisition is used to acquire diagnostic images and to generate a permanent high-quality record of the procedure. Although representing only 5–30 % of the total X-ray tube operation time, approximately 80 % of the total radiation exposure to staff and patients occurs during cine. Significant reductions in exposure can be realised by being aware of when cine is or will be used and applying radiation safety measures accordingly. For example, it is generally not necessary to be as close to the patient during acquisition runs because modern catheters are safer and remote-assisted injectors are now available.
Minimising Radiation Exposure in the Catheterisation Laboratory
The level of radiation exposure in the cath lab can be reduced considerably through the adoption of preventive practices, by employing appropriate physical shielding, by reducing exposure time, and by increasing the distance between staff and the radiation source.
It remains vital that all staff understand the importance of self-monitoring and recognise the risks of radiation. In France, regulations introduced in 2004 mandate two days of training for all doctors and technicians involved in situations where patients are exposed to radiation.
Distance
The intensity of radiation exposure at a given point relates to the distance from the emitting X-ray source through the inverse square law. This means that doubling the distance between the source of scattered radiation (the patient body) and the operator will reduce the exposure by a factor of four. In addition, operator exposure varies according to the beam projection used – left oblique projections are much more unfavourable (in a typical situation where the operator is on the right side of the patient) and craniocaudal angulations increase radiation exposure even more. An angle of 60 ° results in an operator exposure dose threefold higher than an angle of 30 °.9 The second operator or assistant is generally less exposed to radiation than the first operator, but is certainly more at risk than other staff in the room. Compliance with an optimal distance focus intensifier (DFI) value, generally 100 cm, is key to allowing an energy reduction delivered by the X-ray tube of a factor of three.9
There are several techniques available that allow for increasing the distance between the radiation source and the operator, including the use of the ACIST CVi Contrast Delivery System, which is discussed later in this article.
Collimation and Edge Filter
Collimation and edge filter are types of housing placed at the exit of the X-ray tube. Collimation allows a reduction of both patient and staff exposure by narrowing the imaging field of interest. Edge filter allows a partial reduction of the primary beam corresponding to low attenuation parts of the patient’s body, such as the lung. These two options improve image quality and result in a decrease in the energy delivered to the patient.
Shielding
Radioprotective shielding can significantly reduce the level of exposure, if used and maintained appropriately. Protective equipment includes lead aprons, thyroid collars and leaded glasses. A thyroid shield is mandatory to protect the neck. It is recommended that cath lab staff should wear a protective apron of at least 0.5 mm lead equivalence (providing a reduction factor of approximately 100-fold).10 Protective leaded eyewear is recommended because the lens appears to be highly sensitive to exposure.
Lead glasses (0.75 mm lead equivalent) should be worn to counter specific risks such as cataract. These measures, however, do not protect against radiation exposure to the head, arms and legs. Therefore, many cath labs use overhanging lead screens to prevent radiation exposure to the brain. These should be a minimum of 0.5 mm lead equivalence. Suspended lead shields around the cath lab table help to minimise radiation exposure to the legs.
Mobile lead shields provide a further opportunity to reduce radiation exposure for the operator. A newly developed mobile shield (PISAX) is available (see Figure 1).
Time
The length of time during which an individual is exposed to radiation is a significant determinant of risk. On average, the procedure time for a diagnostic coronary angiogram is approximately 30 minutes, and an interventional procedure or electrophysiology/pacing study would take 90–120 minutes. However, the time required for fluoroscopy and cine screening varies greatly depending on the nature of the procedure and the experience of the operator. Every effort should be made by the operating cardiologist in the cath lab to minimise fluoroscopy and cine screening time.
An effective way to reduce the exposure time is adoption of the ACIST CVi Contrast Delivery System. In a study by Brosh et al., a reduction of the fluoroscopy time of 25 % was reported with use of the ACIST CVi system, compared with a manual injection technique.11 Additionally, the three-dimensional (3D) rotational angiography technique can help to reduce fluoroscopy time. In 3D rotational angiography all projections of each coronary artery system are visualised in one cine angiogram during a longer, continuous injection of contrast. One study reported a reduction in radiation dose of 35 % with this technique.12
About the ACIST CVi System
The ACIST CVi system (see Figure 2) was developed to facilitate contrast injection in all angiography procedures. The ACIST CVi system uses the sterile AngioTouch® pneumatic hand controller, allowing the operator to control the flow and volume of contrast media directly from the sterile field. The system allows for precise control of injection volume and timing, leading to a significant reduction in the amount of contrast delivered.11,13,14 The ACIST CVi Contrast Delivery System was adopted by Clinique St Gatien, France, in 2000.
The ACIST CVi Contrast Delivery System allows the operator to stand at a greater distance during imaging, facilitating use of the 2 mm lead equivalent PISAX protection shield while maintaining precise control over the flow and volume of contrast media.
Using ACIST CVi to Improve Radiation Protection
During image acquisition runs, the use of the ACIST CVi injector allows the operator to stand further away from the patient than would be possible with a conventional injection system, thus significantly improving radiation protection. Dr Bar’s group has studied the effect of using the ACIST CVi system on radiation exposure, comparing the radiation exposure of the left hand when using a hand manifold technique and the ACIST CVi contrast delivery technique. In this study, a reduction in radiation dose of 3.4-fold was seen in diagnostic angiography procedures and a 1.7-fold reduction occurred during percutaneous coronary intervention (PCI) procedures (publication in press).
Additionally, the ACIST CVi system facilitates the adoption of 3D rotational angiography, allowing for a safer distance and a consistent flow of contrast during the angiography runs. The adoption of this technique allows for a reduction in contrast and radiation dose.15
Combination Approaches
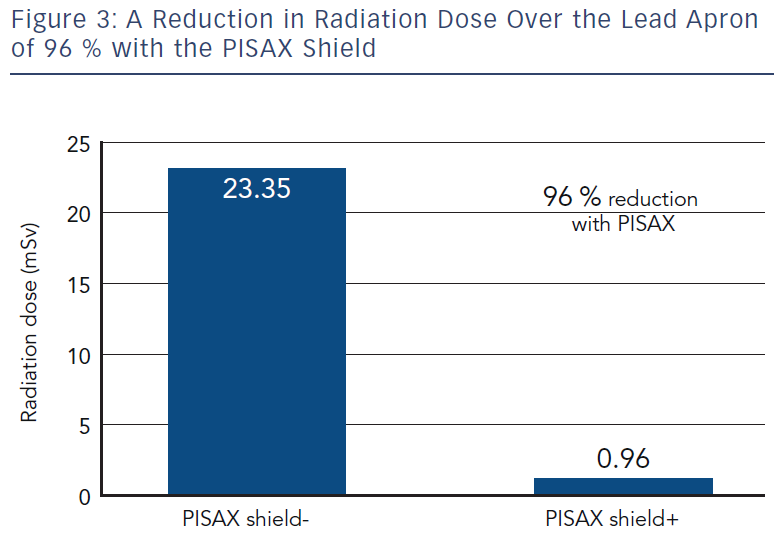
Use of the PISAX radiation shield with the ACIST CVi system is a modern and efficient way of working that can lead to a significant reduction in whole-body radiation exposure. In order to take full advantage of the benefits of the PISAX radiation protection shield, it is required that the operator stand behind the shield during the cine runs, while simultaneously delivering contrast. The ACIST CVi system provides the physician with the option to stand safely behind the shield when contrast is delivered and the angiogram is recorded.
A study was conducted to compare the annual dosimetry results measured outside the lead apron of two interventional cardiologists working with the ACIST CVi system with or without the PISAX radiation shield. Both cardiologists performed more than 500 procedures per year and individual dosimetry results were weighted by their relative activity.
These results show a dramatic reduction of dose to unprotected body parts of staff (arm, head and legs) when the specific mobile 2 mm lead shield PISAX is used together with the ACIST CVi system (see Figure 3).
Conclusions
Interventionists are encouraged to remain vigilant regarding the particularly high level of radiation in the cath lab setting. Preventative measures should be implemented to limit staff exposure, including minimising fluoroscopy and cine time, increasing the distance from the radiation source during imaging, and employing appropriate physical shielding.
The ACIST CVi system can help to reduce radiation dose both to staff and to patients by reducing procedure times, and enables the interventionist to increase their distance from the radiation source (the body of the patient) during image acquisition while maintaining precise control of contrast injection.
A profound reduction in radiation exposure of 96 % was observed when the ACIST CVi system was used in conjunction with the 2 mm lead equivalent PISAX radiation protection shield, which allows the operators to shield themselves during angiography while controlling contrast delivery. This modern combination of devices contributes to making the cath lab safer both for staff and for patients.