The focus of Dr Schäfer’s talk was the impact of complete revascularisation in acute MI cardiogenic shock (AMICS). When considering revascularisation in this context, two methods of percutaneous coronary intervention (PCI) are used: culprit-lesion-only PCI, which involves revascularisation of the lesion involved in the index acute MI; and complete revascularisation, which targets all significant lesions in the coronary tree, not just the culprit lesion.
Recent work from the CULPRIT-SHOCK trial has suggested that outcomes with multivessel PCI are inferior to culprit-lesion-only PCI in terms of 30-day mortality.1 Closer analysis of the results showed that the difference in all-cause mortality between these two PCI methods was 8.2% and that most of this difference can likely be attributed to anoxic brain injury, which was 6.8% higher in multivessel PCI. Brain injury is common in patients who experience cardiac arrest. It has been reported that 50–60% of AMICS patients in clinical studies have experienced cardiac arrest prior to randomisation.1 Dr Schäfer believes that the disproportionate representation of brain injury may be related to the high proportion of resuscitated patients in the trial rather than the cardiogenic shock itself. In fact, in the CULPRIT-SHOCK population, the 30-day mortality due to refractory cardiogenic shock was 8.4% lower for multivessel than culprit-lesion-only PCI.1 In addition, the increased amount of contrast agent and longer procedure duration could have contributed to the adverse outcomes in the multivessel PCI group. Dr Schäfer asserted that outcomes in the multivessel PCI group could be improved by using mechanical circulatory support (MCS).
Specifically, Dr Schäfer presented data from 10 publications showing that installation of MCS and unloading prior to the PCI procedure were consistently associated with improved 30-day mortality outcomes in AMICS patients. Based on the analysis Dr Schäfer’s group performed on 166 real-world AMICS patients from four EU centres, the use of Impella as an unloading strategy during multivessel PCI in AMICS patients significantly reduced mortality in the highest-risk group stratified by the SHOCK-II score.
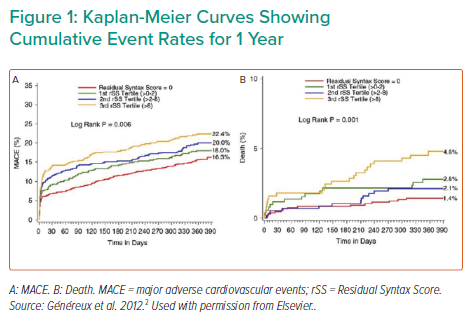
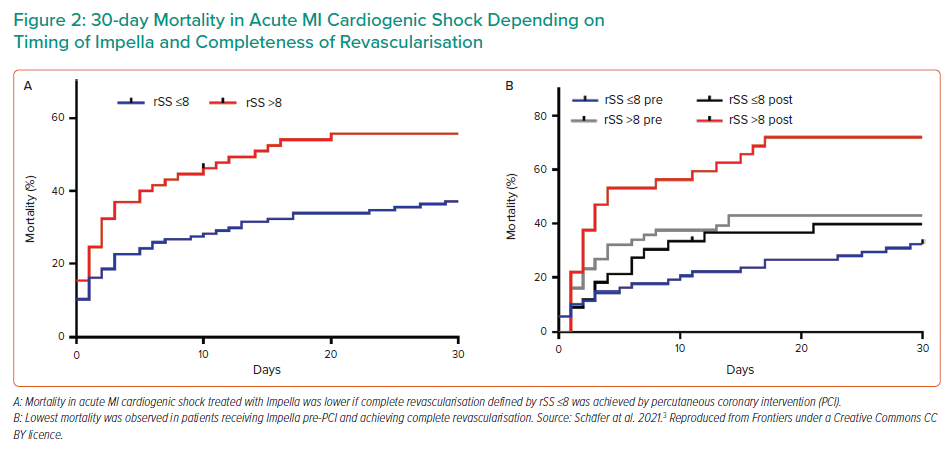
Although assessing complete revascularisation is difficult, the Residual Syntax Score (rSS), which measures the burden of residual coronary artery disease after PCI, is an independent predictor of cardiac death and MI in acute cardiogenic shock PCI patients.2 An rSS <8 indicates complete revascularisation and is associated with significantly reduced rates of major adverse cardiac and cerebrovascular events, as well as improved survival rates (Figure 1). Dr Schäfer and his team used the rSS to investigate the effect of complete revascularisation while on Impella CP support before PCI in AMICS. Mortality rates were significantly reduced among patients who achieved an rSS ≤8 than among patients with an rSS >8 (p<0.0001; Figure 2A). Furthermore, mortality was significantly reduced among patients who received Impella support before versus after PCI for both rSS groups. Together, the data indicate that patients with an rSS ≤8 who received Impella support before PCI had the lowest mortality rates, whereas mortality rates in patients with an rSS >8 who received Impella support after PCI were the highest (Figure 2B).
Dr Schäfer concluded that implanting the Impella CP prior to PCI, with the goal of complete revascularisation while on Impella support, resulted in decreased mortality rates in patients with AMICS.