Cardiovascular diseases (CVD) are the world’s number one cause of death with an estimated 17.9 million deaths per year, representing about 31% of deaths globally. CVDs manifest in various forms including ischaemic heart disease (IHD; either as acute coronary syndrome or chronic coronary syndrome), cerebrovascular disease and peripheral vascular disease. The lesser forms of CVD include heart failure, heart rhythm disturbance (arrhythmias), valvular heart disease, congenital heart disease, cardiomyopathies, aortic aneurysms and venous thromboembolism, with 85% of deaths from CVD worldwide caused by acute coronary syndrome and cerebrovascular disease.1,2 Although IHD is the single most common cause of death globally and its frequency continues to increase, the overall mortality trend in Europe has been steadily decreasing in the past three decades, with the largest declines in the Netherlands and the UK.3
Acute coronary syndrome includes ST-segment elevation MI (STEMI), non-STEMI (NSTEMI) and unstable angina. The relative incidence of NSTEMIs has increased slightly and that of the STEMIs decreased significantly in the US, with long-term mortality in these patients reducing.4,5 Primary percutaneous coronary intervention (pPCI) is the preferred reperfusion strategy for patients with STEMI. STEMI diagnosis and treatment begins from the point of first medical contact and strategies to reduce delays and maximise the efficiency of the pPCI using regional reperfusion strategies have been recommended by various guidelines.6.8
The Belfast pPCI service became operational in April 2007. It offers a 24 hours a day, 7 days a week and 365 days a year service to the catchment areas of Ulster, Downe, Lagan Valley, Antrim, Daisy Hill, Craigavon, Ballycastle and Ballymoney in the UK.9 The service involves nurse-led ECG interpretation undertaken after these have been transmitted electronically to a dedicated email address in conjunction with a pre-alert call to a dedicated telephone line from the Northern Ireland Ambulance Service (NIAS).
With the outbreak of COVID-19 and its subsequent declaration as a public health emergency by the WHO on 30 January 2020, the effect of COVID-19 on healthcare systems around the world cannot be overemphasised.10 As of 27 February 2020, there were confirmed cases within and outside China.11 As the number of cases continued to rise exponentially globally, there were 6,650 cases in the UK when it entered a full national lockdown on 23 March 2020.12 A study from London has shown there was a reduction in admission of patients with STEMIs and that the pPCI pathways can be maintained during the pandemic.13 Similarly, a survey of 3,101 responders from 141 countries and six continents indicated that there was >40% reduction in STEMI admissions during the pandemic and this is also in agreement with the National Institute for Cardiovascular Outcomes Research (NICOR) COVID-19 report.14,15
Historically, about 60% of patients referred to the Belfast pPCI service are appropriately turned down as shown in previous studies.16,17 In light of this, we evaluated the impact of COVID-19 on our pPCI service during the first wave of the pandemic in the UK from 23 March to 9 June 2020. The aim was to find out if there had been a reduction in the number of pPCIs performed and whether there had been any changes to the referrals to the pPCI service which meant patients had been inappropriately turned down.
Methods
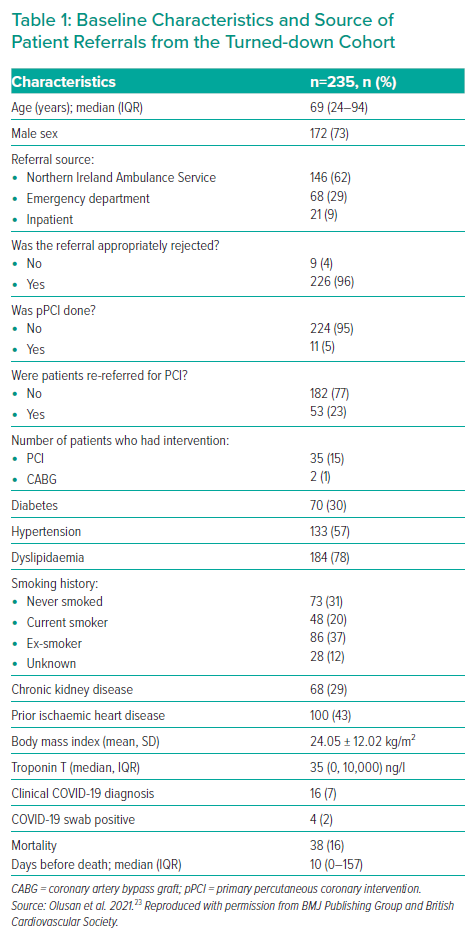
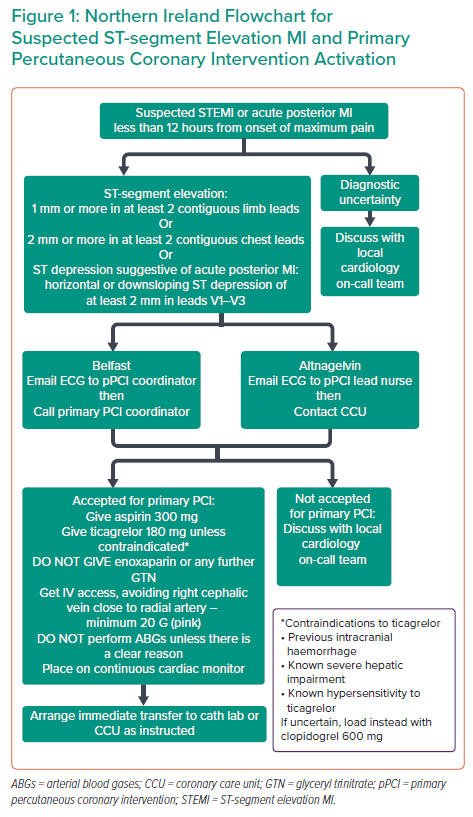
When a patient is referred to the Belfast pPCI service, their ECGs are triaged by the pPCI coordinator who logs the details of referrals and the ECG in a standardised locally agreed Proforma document and a Microsoft Access database. Criteria for acceptance for pPCI are chest pain of <12 hours onset and either ST-segment elevation (1 mm or more in at least two contiguous limb leads; 2 mm or more in at least two contiguous chest leads) or ST segment depression suggestive of acute posterior MI (horizontal or downsloping ST segment depression of at least 2 mm in leads V1–V3). Patients meeting these criteria are immediately transferred to the catheter laboratory (Figure 1). However, patients who are not accepted into this pathway by not meeting the above criteria are advised to be reassessed by the local cardiology team. Furthermore, patients without clear-cut diagnosis of STEMI on ECG, including those with left bundle branch block morphology or paced rhythm, are discussed with either the on-call cardiology registrar or interventional cardiologist before a decision is taken to either accept the referral or turn it down.
This was a retrospective observational study of all referrals to the Belfast pPCI service during the first wave of COVID-19. All ECGs were reviewed with corresponding referral history logged on the database and call log sheets. Supplementary clinical data was collected using the Northern Ireland Electronic Care Record (NIECR) to assess admission location, cardiovascular risk factors (diabetes, hypertension, dyslipidaemia, smoking, high BMI and chronic kidney disease), prior ischaemic heart disease, high sensitivity troponin-T levels, final diagnoses, COVID-19 swab results and mortality. A turndown was deemed inappropriate if the retrospective review of history and ECG demonstrated that the pPCI entry criteria had been met. The number of pPCIs performed was compared with the same period in 2019.
Statistical analyses were performed using Stata/IC 15.1. Continuous variables were expressed as mean alongside standard deviation (SD), median alongside interquartile range (IQR) for parametric and non-parametric variables, respectively. Similarly, categorical variables were expressed as proportion (%) and χ2 or Fisher’s exact tests were used to test for statistical significance. A p-value ≤0.05 showed statistical significance.
Results
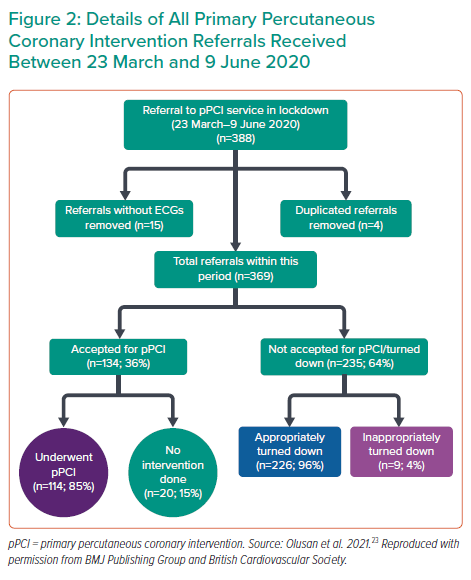
During the 78-day period, a total of 388 patients were referred to the Belfast pPCI service – an equivalent of five referrals per day. Of these, 19 were excluded from analysis owing to duplicated (n=4) and incomplete (n=15) referrals (i.e. without ECGs). Of the 369 patients included in the study, 235 (64%) were turned down for pPCI and 134 patients (36%) were accepted for pPCI.
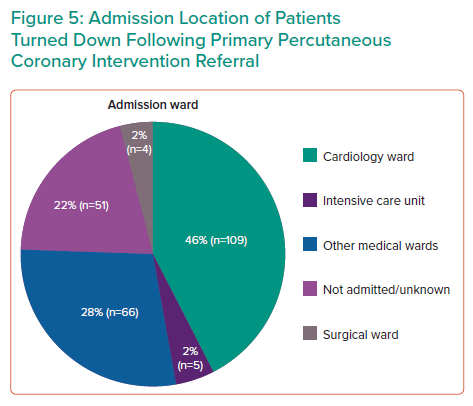
In the accepted cohort, 114 patients (85%) had pPCI to a culprit coronary artery and 20 patients (15%) had no intervention performed. The reasons for no intervention included: takotsubo syndrome (n=3); coronary spasm (n=1); pericarditis (n=4); chronic total occlusion (CTO) (n=3); non-obstructed coronary artery (n=8); and stroke (n=1). In the turndown cohort, nine patients (4%) were inappropriately turned down for pPCI which was 2.4% of all referrals (Figure 2). The median age of patients from the turndown cohort was 69 years with an IQR 24–94 years and 73% were men. The vast majority of turned down referrals (n=146; 62%) were received from NIAS (Table 1) and 46% (n=109) of the patients who were turned down were admitted to cardiology wards (Figure 3).
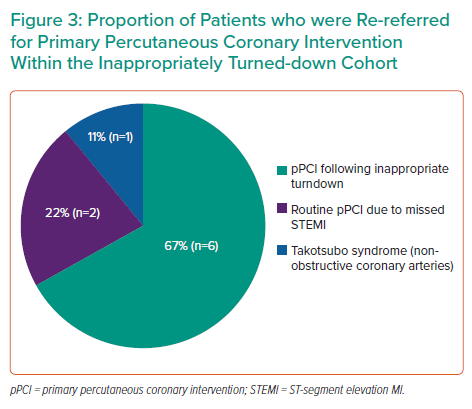
Of the nine patients who were inappropriately turned down, six subsequently had a pPCI performed to culprit vessels following re-referral from the local district general hospital. These include pPCI to the left circumflex artery (LCx) for a lateral STEMI (n=1); pPCI to the vein graft to obtuse marginal artery for a posterior STEMI (n=1); pPCIs to the left anterior descending artery (LAD) for an anterior STEMI and an initially missed anterior STEMI (n=2); pPCI to the left main coronary artery (LMCA), LAD and LCx for an anterior STEMI (n=1); and pPCI to the right coronary artery (RCA) for an Inferior STEMI (n=1). Two patients from the inappropriately turned down cohort had missed STEMI, each of whom had a routine PCI to LAD for anteroseptal STEMI and routine PCI to LMCA and LCx for posterior STEMI on day 9 and day 4, respectively, after intial referal. The remaining patient from the inappropriately turned down cohort was diagnosed with takotsubo syndrome after coronary angiography demonstrated non-obstructive coronary arteries (Figure 3). Furthermore, there were four cases of NSTEMIs with subsequently evolving ECG changes and ongoing ischaemia that required pPCI (two RCA, one LCx and one vein graft to the obtuse marginal artery). One patient who was initially appropriately turned down subsequently developed anterior STEMI and required pPCI to LAD.
Further analysis of the appropriately turned down cohort demonstrated that three patients had ST-segment elevation on lead aVR associated with inferolateral ST-segment depression. These were appropriately turned down because they did not meet the pPCI pathway activation criteria. Two of the three patients had cardiovascular mortality (aged 85 and 94 years) and the third patient (aged 65) had a coronary artery bypass graft (CABG).
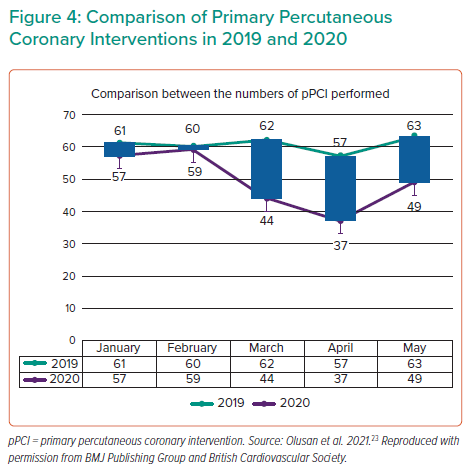
The impact of COVID-19 on referrals to our pPCI service during the first wave of the pandemic was then assessed to see if there were any referrals turned down due to COVID-19. There were 16 patients with clinically suspected COVID-19, four of whom were swab positive for COVID-19 infection. No patient was turned down because of COVID-19. In 2020, there was a 29% reduction (130 versus 180) in the number of pPCIs performed in the 3 months from March to May in comparison with the previous year (Figure 4).
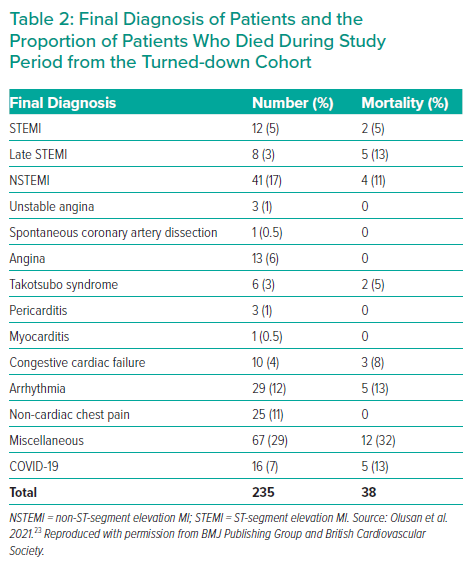
In the appropriately turned down cohort, the final diagnosis was cardiovascular in 127 patients (53%), non-cardiac chest pain in 25 patients (11%) and miscellaneous in 67 patients (29%), while COVID-19 was diagnosed in 16 patients (7%; Table 2). The miscellaneous diagnoses included gastritis, acute kidney injury, myositis, hepatosplenic abscess, transient ischaemic attack, gastroenteritis, infective exacerbation of chronic obstructive lung disease, vestibular neuritis, subarachnoid haemorrhage, diabetic ketoacidosis, pneumonia, seizure, septic shock, upper gastrointestinal bleeding, overdose, colitis, pancreatitis, anaemia, liver tumour, prostate cancer, metastatic colon cancer, alcohol intoxication and renal lithiasis. The admission ward of patients within the turndown cohort was examined and about 46% of patients were admitted to a cardiology ward (Figure 5).
The 1-year mortality rate of the 235 turned-down patients was 16% (n=38) of which about 55% (n=21) was due to a cardiovascular cause – STEMIs (n=2), late STEMIs (n=5), NSTEMIs (n=4), takotsubo syndrome (n=2), congestive cardiac failure (n=3) and ventricular arrhythmias (n=5); 13% (n=5) were due to COVID-19 and 32% (n=12) were due to the miscellaneous causes listed above (Tables 1 and 2). There were no deaths recorded within the inappropriately turned down patients. We assessed the effect of inappropriately turned down referrals on mortality, but there was no statistically significant association (p=0.51, Fisher’s exact).
The association between sex and mortality was also assessed using the Fisher exact test, and this demonstrated a significant association between female sex and mortality (female 14/45 [31.1%]) versus men 24/145 [16.6%], p=0.042). There was no difference noted between the sexes in relation to clinical COVID-19 diagnosis (p=0.16).
The association between clinical COVID/swab-positive COVID-19 and cardiovascular risk factors, such as diabetes, hypertension, dyslipidaemia, smoking, chronic kidney disease and past history of ischaemic heart disease, was examined, but the only statistically significant association was found between diabetes and clinical COVID-19 diagnosis (χ2 test, p=0.03). There was a statistically significant association between diabetes and mortality (χ2 test, p=0.05).
Discussion
This study provides contemporary data of the impact of COVID-19 on the pPCI service during the first wave of the pandemic in the Belfast region. A higher proportion of referrals did not meet the criteria for pPCI from which 4% were inappropriately turned down. Of those, 89% had pPCI to the culprit vessel. A number of these patients had clinical reasons for being declined initially: resolution of ST-segment elevation; three-vessel coronary disease including known CTO-LAD (patient was awaiting CABG). The proportion of turned-down referrals is similar to published data from previous studies within the UK.16–18 About half of those who were appropriately turned down had a final cardiovascular diagnosis.
A higher proportion of referrals were received from paramedics (NIAS) and this is similar to what is expected within the general population. A culture of paramedics’ upskilling in the early detection of STEMI on ECG and subsequent referral to the pPCI pathway has been developed over the years, in line with stipulated guidelines.6–9 Of those patients excluded from this study, 15 were due to non-transmission of ECGs at the time of referral, which could be improved upon.
COVID-19 significantly reduced the number of pPCIs performed during the first wave of the epidemic at the Belfast trust and this is in agreement with findings in other studies; nevertheless, no referrals were inappropriately turned down because of COVID-19 at our regional centre.13–14,19
ST-segment elevation in at least two contiguous leads has been a universal criteria for STEMI diagnosis as stipulated by recommended guidelines which is reflected in the Belfast pPCI activation pathway (Figure 1). 6–8 There was a 67% (n=2) mortality in patients presenting with ST-segment elevation in lead aVR and 33% (n=1) had CABG. It is well recognised that ST-segment elevation in aVR denotes significant left main coronary artery disease or occlusion.20–22 Although these patients do not meet criteria for pPCI they can be referred for emergency PCI after initial cardiology assessment in the referring hospital.
The study’s strengths included examining first referrals to the Belfast pPCI service not just from paramedics but also those from emergency department and inpatient wards which gives an overview of all referrals to the service. Although there were concerns that COVID-19 transmission could have affected the decision-making of the pPCI coordinators, there were no cases turned down because of COVID-19. The use of electronically transmitted ECG helped ensure that all transmitted ECGs could be retrospectively analysed to ascertain whether the referrals were appropriate. The availability of a national electronic healthcare database, NIECR, helped ensure the tracking of most patients to ascertain their final diagnoses and mortality.
There are some limitations to this study. As with all observational studies, we cannot fully eliminate the risk of bias; however, we ensured that all electronically transmitted ECGs assessed in this study were reviewed by four different cardiology specialist registrars individually, which helped eliminate bias to some extent. A few of the patients had missing data, e.g. nine of the patients had no available health and social care number, which meant we were unable to track this subset of the cohort, but this was not significant enough to invalidate this study. This study was unable to ascertain a statistically significant association between COVID-19 and known comorbidities for COVID-19 except for diabetes, which may be because the few patients in the study with COVID-19 were among this cohort.
Learning points gained during the first wave of COVID-19 which have influenced our service during subsequent waves include: ensuring patients seek help early and feel safe to be admitted to hospital to avoid late presentation and increased mortality; turned-down patients with alternative diagnoses to STEMI (such as NSTEMIs, takotsubo syndrome, congestive cardiac failure and ventricular arrhythmias) should be assessed by a specialist team and treated appropriately to reduce mortality in these cohorts.
Conclusion
During the first wave of COVID-19 there was a significant reduction in the number of pPCIs performed. This was not due to an increase in referrals being inappropriately turned down and no patient was turned down because of COVID-19. Of the patients whose referrals were turned down, the majority (53%) had a final cardiovascular diagnosis unrelated to STEMI and 1-year mortality in this group was significant.
Measures to ensure patients seek help early and feel safe in a hospital environment in addition to specialist team review of turned-down patients will help mitigate mortality.
Clinical Perspective
- COVID-19 significantly reduced the number of pPCIs performed during the first wave, although there were no patients turned down for pPCI due to COVID-19.
- Measures to reduce 1-year mortality include ensuring that patients seek help early to avoid late presentation and those with alternative diagnoses obtain specialist help and follow-up.
- It is well recognised that ST-segment elevation in aVR denotes significant left main coronary artery disease or occlusion. Although these patients do not meet criteria for pPCI they can be referred for emergency PCI after initial cardiology assessment in the referring hospital.